With the advent of a new year, many people aim to shed outmoded habits in favor of improved lifestyles. In the increasingly data-driven medical community, the new year brings three new, highly-specific screening codes for Human papillomavirus (HPV). This refinement advances patient care-the prior code set lacked a distinct code to note the precise gene linked with HPV, high- and low-risk. In terms of lab workflow, the new codes hinge coding decisions on more than methodology.
The old CPT codes differentiated HPV testing based on assay technique (87620 for direct probe, 87621 for amplified probe, and 87622 for quantification). As of January 1, 2015, these codes have been eliminated and replaced with new codes (87623, 87624, and 87625) that differentiate HPV genotypes by cancer risk.
"The most recent national guidelines for cervical cancer screening and management recommend only testing for high-risk HPV genotypes," says Michael R. Henry, MD, director, General Cytopathology Laboratory, Department of Laboratory Medicine and Pathology, Mayo Clinic, and medical director of the Cytotechnology Program within the Mayo School of Health-Related Sciences. "There is currently no role for testing for low-risk genotypes for this purpose."
"The FDA recently approved primary high-risk HPV screening with cytology reflex testing," Henry says. "In this scenario, women who are high-risk HPV negative do not need cervical cytology. If they are HPV-16 or -18 positive, colposcopy and biopsy are recommended, and if they are high-risk HPV positive HPV, the recommendation is for reflex Pap cytology. The ability to separate out the different types of HPV testing allows us in the laboratory to fulfill all of these new diagnostic and screening techniques." Henry is a consultant in the division of anatomic pathology and an associate professor of laboratory medicine and pathology at Mayo Clinic. He is also the current president of the American Society of Cytopathology.
HPV genotyping, used alongside an abnormal cytology report or for follow-up, helps detect high-risk genotypes linked with onset of cervical cancer (such as HPV-16 and HPV-18). HPV-16 and HPV-18 genotyping findings can help guide clinicians whose patents have high-risk HPV with negative Pap smear results.
"Most FDA-approved, HPV genotyping assays are focused on identifying the high-risk HPV genotypes," says Omai Garner PhD, D(ABMM), assistant clinical professor, associate director, Clinical Microbiology, UCLA Department of Pathology and Laboratory Medicine, UCLA Health System, Los Angeles. "These assays typically screen using a multiplex, PCR-based, nucleic acid amplification test (NAAT). The new codes allow labs to charge and release results specifically identifying the HPV to genotype. This is critical for patient care."
All three of the new codes crosswalk to 87621.
The new codes are as follows:
• CPT code 87623 refers to low cancer risk, genital wart-associated HPV genotypes (6, 11, 42, 43, and 44).
• CPT code 87624 refers to high cancer-risk HPV genotypes (16, 18, 31, 33, 35, 39, 45, 51, 52, 56, 58, 59, 68).
• CPT code 87625 refers to the most common high cancer-risk HPV genotypes seen in the United States (16, 18, and 45).
If your lab is mulling what to do when a physician calls with a primary screen, Garner says it really is going to depend on the clinical suspicion of the physician. "In most cases, that physician wants a Pap smear and screen for the presence of a high-cancer risk HPV," he says. "At that point, the new CPT codes allow a lab to specifically bill and test for those genotypes (CPT codes 87624 and 87625). Genital wart testing (87623) is not typically performed in a clinical microbiology lab-it is usually performed by histopathology."
Christopher Watt, MD, PhD, assistant professor of clinical pathology and laboratory medicine, associate director, Molecular Pathology, Department of Pathology and Laboratory Medicine, Hospital of the University of Pennsylvania, Philadelphia, and Debbie Nielsen, BA, MP(ASCP), manager, Molecular Pathology, say the new CPT codes have not altered the workflow in their laboratory.
"Currently, only Roche has an HPV assay approved by the FDA for first-line primary screening in women 25 years and older," Watt says. "Thus, any discussion with a provider would need to focus on the local availability of a suitable assay for a primary screen." The referenced test is the cobas HPV Test, a qualitative multiplex assay that simultaneously detects 14 high-risk HPV types and provides specific genotyping information for HPV Types 16 and 18, and at the same time detects the other 12 high-risk HPV types in a pooled result.
This is the first article in a series about HPV testing.
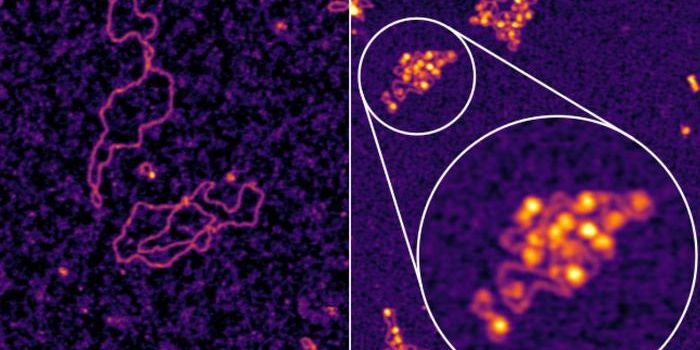
Top Image: Electron micrograph of a negatively stained human papilloma virus (HPV). [Photo credit: Laboratory of Tumor Virus Biology/National Cancer Institute]
HPV is a small, nonenveloped, double-stranded DNA virus, with a genome of about 8,000 nucleotides. More than 118 types of HPV exist, with some 40 HPVs infecting the human anogenital mucosa. About 14 of these types are considered to be high risk for development of cervical cancer and its precursor lesions. HPV types 16 and 18 have been deemed the genotypes most closely linked with progression to cervical cancer. HPV-16, the most carcinogenic, is linked with about 60 percent of all cervical cancers. Persistent infection with HPV is the chief cause of cervical cancer and its precursor cervical intraepithelial neoplasia, and the presence of HPV has been implicated in more than 99 percent of cervical cancers worldwide. [Source: Mayo Clinic/Mayo Medical Laboratories]



![[Guide] 7 Strategies to Boost Laboratory Collaboration](https://d3bkbkx82g74b8.cloudfront.net/eyJidWNrZXQiOiJsYWJyb290cy1pbWFnZXMiLCJrZXkiOiJjb250ZW50X2FydGljbGVfcHJvZmlsZV9pbWFnZV83YzBjZWIwM2Y5YzI4MmFlYzBhZDZhMTcyNTQ1ZGU3YmE4Y2MzMDYyXzUxNDkuanBnIiwiZWRpdHMiOnsidG9Gb3JtYXQiOiJqcGciLCJyZXNpemUiOnsid2lkdGgiOjcwMCwiaGVpZ2h0IjozNTAsImZpdCI6ImNvdmVyIiwicG9zaXRpb24iOiJjZW50ZXIiLCJiYWNrZ3JvdW5kIjoiI2ZmZiJ9LCJmbGF0dGVuIjp7ImJhY2tncm91bmQiOiIjZmZmIn19fQ==)