Bird Flu Spreads to Dairy Cows & Is Detected in Raw Milk
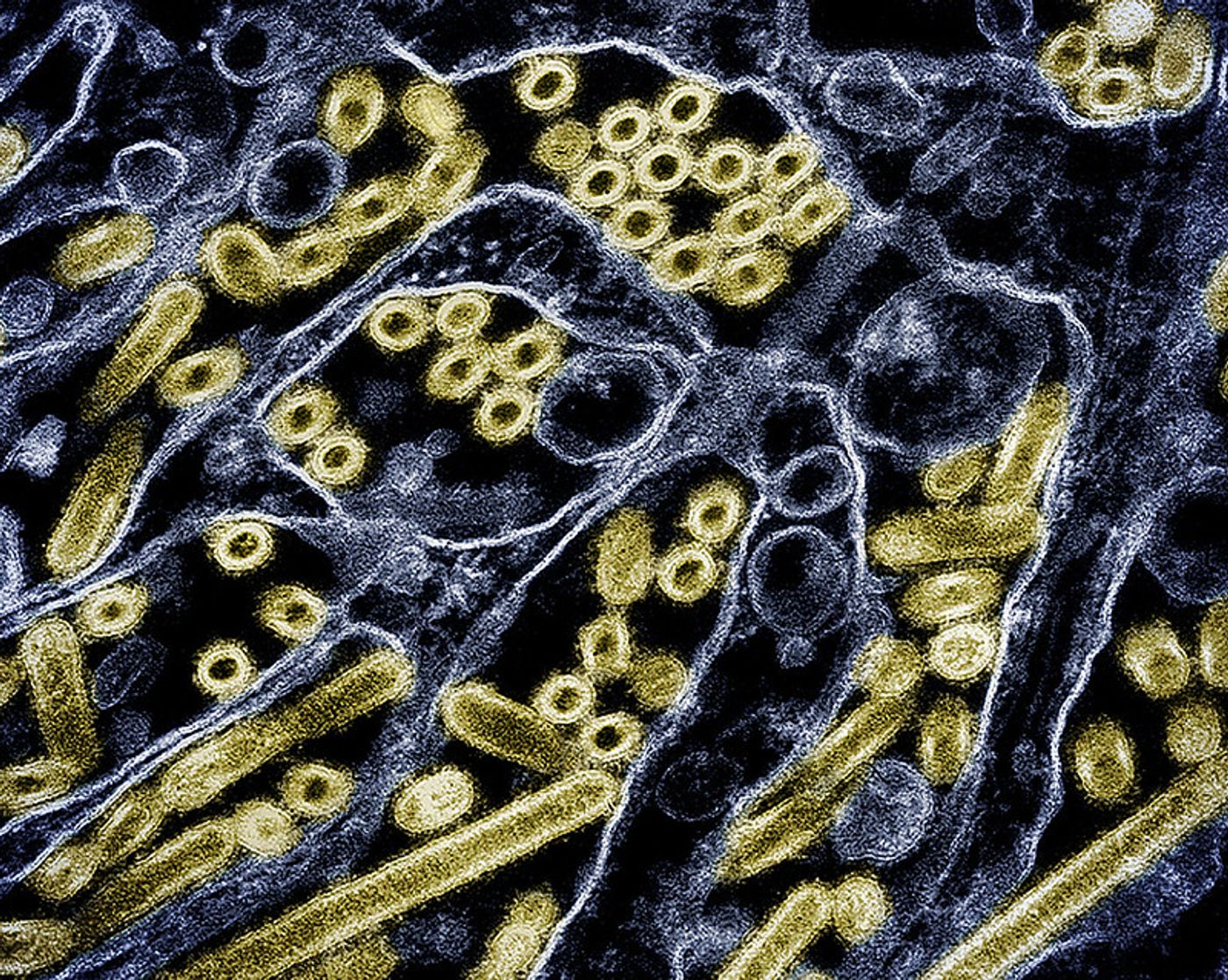
The US Centers for Disease Control and Prevention (CDC) is tracking H5N1, an avian influenza virus that has wreaked havoc on bird populations around the world for several years, and has spilled over into other animals as well. On May 22, 2024, the CDC announced that a second US dairy worker has been confirmed to have an H5N1 infection; this case has occurred in Michigan while the first case of H5N1 in a US dairy worker was confirmed in Texas a few months ago.
Most scientists still consider the risk to the general public to be low. The H5 subtypes of bird flus are usually not good at replicating in the human upper respiratory tract, and as such, they are not currently capable of human-to-human transmission. When humans are infected, it is because they have come into direct contact with an infected animal.
People who work with livestock or other animals are greater risk of H5N1 infection than the general public, and should consider taking as many precautions as possible, as recommended by the CDC.
Experts have stressed, however, that it will still be crucial to monitor this virus, because we cannot possibly know what will happen as it continues to spread and evolve.
The U.S. Department of Agriculture (USDA) is also now trying to reduce the spread of H5N1 in cows, but many scientists think that these measures are too little, too late. While new regulations stress that infected cows can no longer be transported from one state to another, the virus has already been detected in cows in nine states, and widespread testing is not curently being conducted.
The outbreak in dairy cows may have started as long ago as October 2023, and recent research assessing milk, and another study investigating wastewater, has suggested H5N1 is already widespread in US dairy cows.
Some companies are now attempting to develop as vaccine that can be used in cows to prevent H5N1, but there are many challenges, including restrictions involving H5N1 research, which must take place in a in biosecurity level-3 (BSL-3) labs. There are not many of those labs, and even fewer that can handle cows as research subjects. The USDA is now developing a cow model at a facility in Iowa.
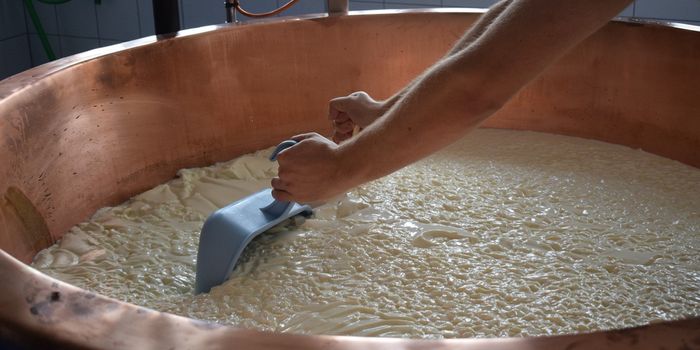
More could still be done to prevent further spread, scientists have suggested. “At milk processing plants, every incoming tanker load of milk is checked for adulterants, including antibiotics, and quality and safety standards,” veterinarian Kay Russo, who helped detect H5N1 at dairy farms for the first time, told Science. If these same standard were applied to H5N1, we would understand “the pervasiveness of this virus almost overnight.”
It's difficult to know what might happen to dairy workers who get infected, because many who get sick may never be tested or seen by a doctor. There may also be many asymptomatic cases.
So is milk safe to drink? Right now, it looks like pasteurized milk is safe to drink. However, unpasteurized or so-called raw milk contaminated with H5N1 did infect mice who consumed the drink in a study that was recently reported in the New England Journal of Medicine. In as little as one day after consuming the tainted milk, the mice showed signs of illness like lethargy. The researchers also found high levels of the virus in the respiratory tracts of the mice, which were all euthanized four days after exposure so they could be analyzed.
Refrigeration also barely affected the level of the virus in the raw milk itself, causing the levels to go down only slightly. In pasteurization, liquids are heated rapidly, which kills most biological contaminants.
"Don't drink raw milk: that's the message," senior study author Yoshihiro Kawaoka of the University of Wisconsin–Madison told the New York Times.
Sources: CDC, Science, New England Journal of Medicine