Study Shows Probiotics Provide a Questionable Benefit at Best
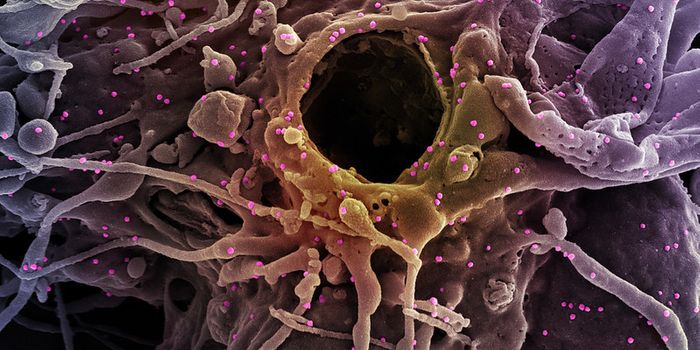
Probiotics have entered the mass market as both food additives and supplements, and they have been touted as a health benefit. There is not a lot of research to support those claims, however, and new work suggests that they may not be exerting any effects on the bacteria that live in the human gut. We normally have a vast number of microorganisms living in our gastrointestinal (GI) tract, and they can have a powerful effect on health. Incredibly, the researchers found that probiotics interfere with the recolonization that happens in the gut after antibiotics disrupt or destroy the microbiome. This work has been reported in two papers in Cell.
"People have thrown a lot of support to probiotics, even though the literature underlying our understanding of them is very controversial; we wanted to determine whether probiotics such as the ones you buy in the supermarket do colonize the gastrointestinal tract like they're supposed to, and then whether these probiotics are having any impact on the human host," said senior author Eran Elinav, an immunologist at the Weizmann Institute of Science in Israel.
"Surprisingly, we saw that many healthy volunteers were actually resistant in that the probiotics couldn't colonize their GI tracts. This suggests that probiotics should not be universally given as a 'one-size-fits-all' supplement. Instead, they could be tailored to the needs of each individual,” Elinav added.
Instead of taking the usual route for microbiome studies, which is to analyze bacterial genes in feces, this study assessed gut strains directly. Upper endoscopies and colonoscopies were performed on 25 patients, first to measure baseline levels of bacterial strains. The volunteers were placed in two groups; one took probiotic strains and the other ingested placebos. They underwent the procedures a second time and were monitored for two months.
Some people were successfully colonized by the probiotics - in the so-called persister group. In the resister group, however, there was no growth because those guts had expelled the probiotics. In addition, the team determined that an individual's gut gene expression profile could accurately predict whether they would be a persister or resister.
Their work also showed that fecal sampling might not be an accurate way to monitor gut microbes; microbiome functioning correlated, but only partially, with stool samples.
Related: Use of Probiotics Linked to Severe Bloating, Brain Fog
"Although all of our probiotic-consuming volunteers showed probiotics in their stool, only some of them showed them in their gut, which is where they need to be," explained Segal. "If some people resist and only some people permit them, the benefits of the standard probiotics we all take can't be as universal as we once thought. These results highlight the role of the gut microbiome in driving very specific clinical differences between people."
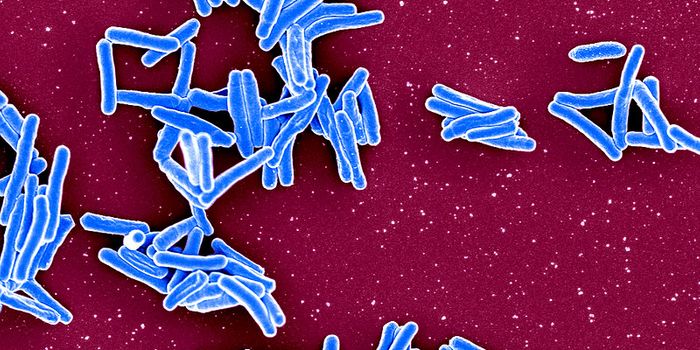
In a second study, three groups of patients were given a round of antibiotics, then given either probiotics, a fecal microbiome transplant, or nothing at all. Following antibiotic treatment, the gut was open for colonization, and standard probiotics restored gut bacteria faster than those recovering with no help, but that fast recovery came at a price. In that probiotic group, the person’s normal microbiome was not re-established, and their gene profile was altered. The group that received the fecal transplant (from their own sample) was able to quickly return to normal, however.
"Contrary to the current dogma that probiotics are harmless and benefit everyone, these results reveal a new potential adverse side effect of probiotic use with antibiotics that might even bring long-term consequences," Elinav said. "In contrast, replenishing the gut with one's own microbes is a personalized mother-nature-designed treatment that led to a full reversal of the antibiotics' effects."
"This opens the door to diagnostics that would take us from an empiric universal consumption of probiotics, which appears useless in many cases, to one that is tailored to the individual and can be prescribed to different individuals based on their baseline features,” Segal concluded.
Sources: AAAS/Eurekalert! via Cell Press, Cell Zimora et al, Cell Suez et al