Immune Stem Cells Treat the Most Common Type of Liver Cancer
There are more multiple causes of hepatocellular carcinoma (HCC) and more than five approaches to treating it. Well, add one more to the list. Combining stem cell science and immunotherapy techniques, Kumamoto University scientists might be on the brink of the most effective treatment yet, for a condition that is the most common form of liver cancer and which has an unfortunately high mortality rate.
Several conditions increase a person’s risk of developing HCC: hepatitis B, hepatitis C, cirrhosis, obesity, diabetes, iron buildup in the liver, exposure to aflatoxins produced by fungi on some types of food. Radiation, chemotherapy, cryo- or radiofrequency ablation, resection, and liver transplants are all options doctors might consider to treat a person with HCC, but the five-year survival rate is still less than 50 percent, and that’s just for localized cases of cancer, where the liver tumors have not yet metastasized.
A new study, published in the Journal of Hepato-Biliary-Pancreatic Sciences, might be the beginning of a completely new option to improve the five-year survival rate for HCC.
Induced pluripotent stem cells (iPSCs) are cells that are useful in experimental medicine because of their innate ability to become multiple cell types. In the present study, researchers designed immune cells derived from iPSCs, specifically immune cells that produce a protein called interferon-beta (INF-B).
INF-B is recruited by the immune system for two reasons: antiviral abilities and two different types of antitumor activity. Despite their antitumor activity, INF-B proteins cause several problems when implemented into anti-cancer therapies, including accelerated inactivation, poor tissue penetrations, and toxicity.
Kumamoto researchers saw a way around these roadblocks, developing a method to design cells that provide all of the benefits of a INF-B anti-cancer approach without all of the problems and negative side effects: iPSC-derived proliferating myelomonocytic cells (iPS-ML cells).
iPS-ML cell activity resembles the activity of another type of immune cell, tumor-associated macrophages (TAMs). Along with regulatory T cells, TAMs are the primary tumor-promoting immune cells in the tumor microenvironment. With iPS-ML cells appearing to be also capable of promoting tumors, Kumomoto researchers quickly realized them to be the perfect vessel for “sneaking” INF-B into the the tumor microenvironment.
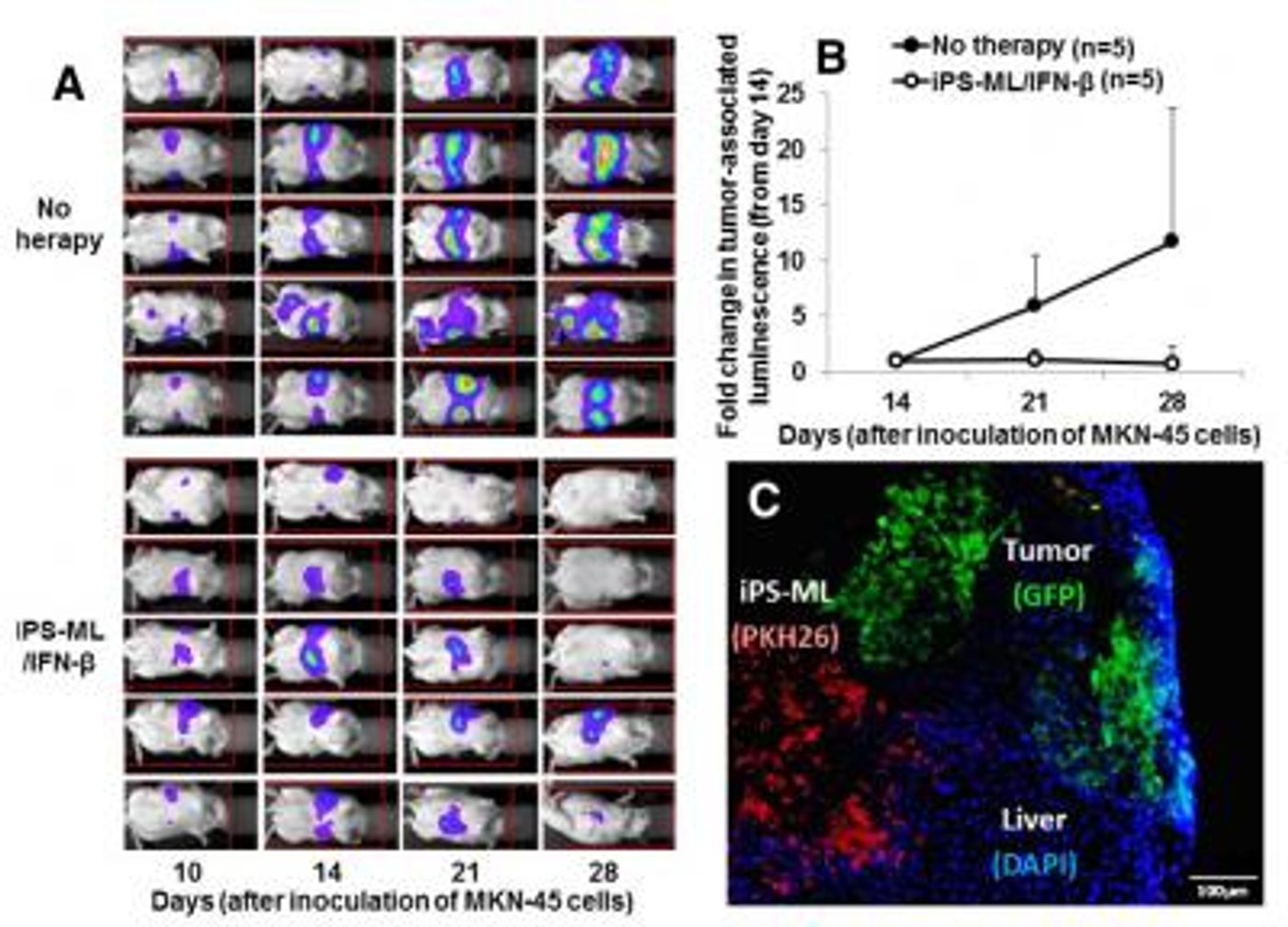
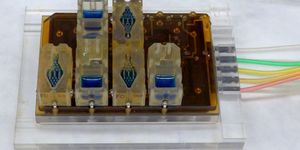
The image above is adapted from the Kumamoto University study results: (A) Bio-imaging analysis to evaluate the therapeutic effect of iPS-ML producing IFN-β on metastatic liver cancer. (B) Quantification of the image data shown in A. (C) Histological data indicating migration of iPS-ML (PKH26, red) into intrahepatic tumor tissues (GFP, green). Credit: Associate Professor Satoru Senju
A mouse study quickly confirmed the potential of iPS-ML/INF-B cells. They found that mice livers with tumors had higher levels of IFN-B than livers without tumors. This is because iPS-ML/IFN-B cells did not penetrate not-tumorous livers, instead they remained on the surface of the healthy organs.
Additionally, they found that IFN-B levels in liver tumors one to three days after the initial injection of iPS-ML/INF-B were high enough to inhibit proliferation or even cause death of tumor cells.
“iPS-cell derived, IFN-β expressing myeloid cells should be beneficial for many cancer patients," said research leader Dr. Satoru Senju. "If it is determined to be safe for human use, this technology has the potential to slow cancer progression and increase survival rates.”
Sources: American Cancer Society, Cellular and Molecular Immunology, Kumamoto University