B cells, which are mostly known for antibody production in the face of invading pathogens, provide another function in the form of marginal zone B cells in the spleen, new findings from the University of Tsukuba reveal.
In response to an endotoxin specific to Gram-negative bacteria called lipopolysaccharide (LPS), B cells of the marginal zone in the spleen exacerbate the inflammatory response to a dangerous level that can lead to inflammation of the entire body system, a condition called sepsis.
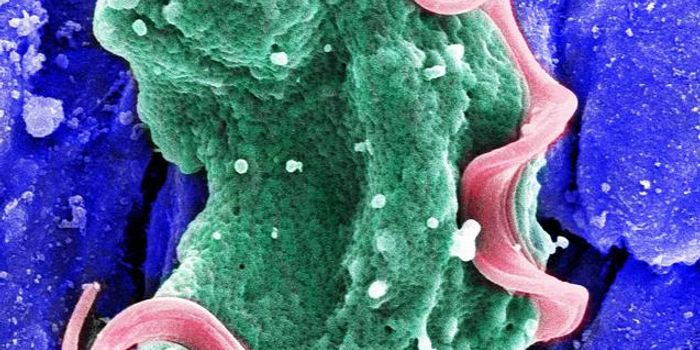
Gram-negative bacteria include
Klebsiella, Acinetobacter, Pseudomonas aeruginosa, and Escherichia coli, and their identifier comes from a common laboratory technique using different chemicals to differentiate between two main types of bacterial organisms that have different cell wall characteristics. Gram-negative bacteria differ from their Gram-positive partners in crime because of their thin layer of peptidoglycan in their cell wall. Gram-negative bacteria are also becoming increasingly resistant to many currently available antibiotics and the Centers for Disease Control and Prevention (CDC) have many guidelines and investigations under way to fight back against multiple-drug resistance.

Marginal zone B cells produce chemokines and cytokines, chemical messengers with different responsibilities. Specifically, marginal zone B cells produce a pro-inflammatory cytokine called interleukin-6 (IL-6). The marginal zone of the spleen separates circulating blood from the surrounding lymphoid tissue, serving to screen for antigens in the bloodstream recognizable by the resident population of lymphocytes.
The researchers from the University of Tsukuba designed a study to understand precisely how marginal zone B cells and IL-6 work to cause sepsis with the hopes of discovering a new way to prevent the transition of sepsis into systemic inflammatory response syndrome (SIRS), which often leads to death.
Tsukuba researchers started by injecting mice with LPS from
E. coli, and they immediately saw increased resistance and survival in mice who had zero marginal zone B cells, as compared to mice with a normal population of marginal zone B cells.
They continued with manipulation of IL-6 activity instead of removing the marginal zone B cells altogether. Compared to blocking IL-6 function just before LPS injection, scientists found that blocking IL-6 function a few hours after injection provided better protection and survival for mice, as compared to control mice with unaltered IL-6 activity.
The researchers also found a third player in the exacerbation of the inflammatory response to LPS: toll-like receptor 4 (TLR4). TLRs of all kinds are present in kinds of organisms, including humans. These receptors play a vital role in “pathogen recognition and activation of innate immunity.” In this study, TLR4 was shown to be required for IL-6 production, and the Tsukuba researchers observed that LPS directly stimulates the marginal zone B cells to produce IL-6 through TLR4.
Lastly, the researchers also studied Fcα/µR because of its expression on lymphoid tissue immune cells and marginal zone B cells. Fcα/µR is an antibody receptor that binds immunoglobulin (Ig) M with high affinity and IgA with a “10-fold lower affinity.” Mice, again with injection of LPS, with deficient levels of Fcα/µR showed decreased production of IL-6 from their marginal zone B cells in response to LPS injection, as compared to control mice.
A “physical association with Fcα/µR was required for forming the TLR4 complex and IL-6 production in response to LPS,” said corresponding author Akira Shibuya, PhD.
Could targeting IL-6 activity for patients at risk for sepsis be a new treatment option to be considered for development? Or perhaps targeting Fcα/µR or even marginal zone B cells directly? Whether it’s one of the three players that is targeted for sepsis treatment or a combination of all three, it is clear that the researchers from the University of Tsukuba are well on their way to developing new therapies for sepsis.
Their study was recently published in the journal
Nature Communications.
Sources:
University of Tsukuba,
CDC,
Microbial Life,
NIH,
Immunobiology