First Animal Model with a Complete Human Immune System
Medical researchers have used animals, particularly mice, to mimic disease and study biological phenomena. The origin of mice as a standard model system for scientific research can extend back to the 1700s when people recorded how they domesticated and bred mice. This early mouse husbandry led to varieties of mice that would eventually be bred to use in the laboratory. In the early 1900s, different scientists recognized the benefit of using mice to study mechanisms of disease. Interestingly, a major advantage to using mice is due to the fact that their anatomy, physiology, and genes are similar to humans. The use of mice generated useful scientific knowledge without having to use human test-subjects. However, unlike their ancestors, laboratory mice have the same genetic makeup.
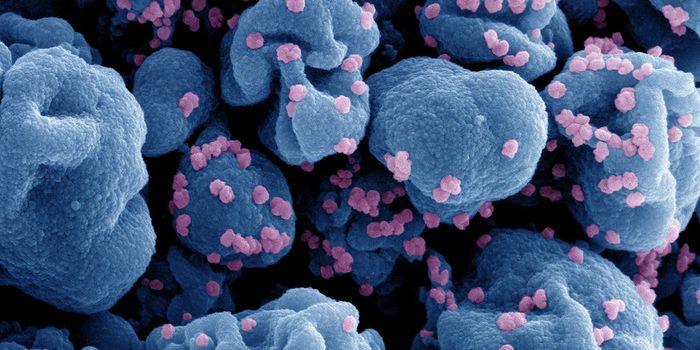
While work in mice is not completely translational to humans, scientists have previously designed different mouse models to better mimic human physiology. The genetic signature of mice can be easily modified to study specific targets that could translate to humans. For example, mice that partially mimic human disease are referred to as humanized mice. The first humanized mouse was created in the 1980s to study human immunodeficiency virus (HIV). Currently, there are many other types of humanized mice, such as patient-derived xenograft (PDX) models, which allow mice to grow human tumor cells. This humanized model is ideal to test novel therapies to determine if the treatment will be effective in the clinic. Although, mouse models are improving, scientists are still working to improve translational feasibility.
A recent article from Nature Immunology, by Dr. Paolo Casali and his team, generated for the first time a mouse that mimics the complete human immune system. Casali is the Ashbel Smith and Distinguished Research Professor at the Long School of Medicine, UT Health San Antonio. Casali’s work focuses on genetic mechanisms that influence antibody response and immune memory in the presence of disease. He utilizes cutting-edge technology to develop different genetic models, cell culture systems, and humanized mice.
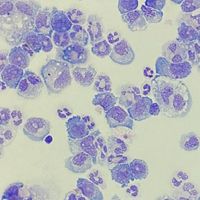
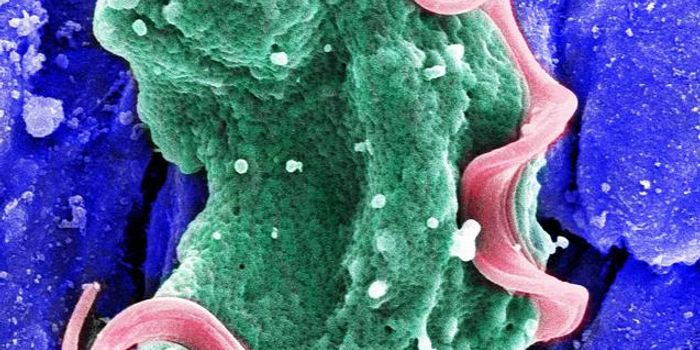
Casali and others demonstrated that their generated humanized mouse had a complete human immune system and human-like gut microbiota, which was able to elicit an antibody response. This is a breakthrough in medical science as it allows us to feasibly predict vaccine efficacy. The goal of creating this mouse was to overcome limitations of current humanized mouse models and to more accurately model immune response. One limitation includes partial human immunity, which leads to ineffective immune responses. This makes the discoveries in mice less translational to improve disease modeling, and develop vaccines and other effective immunotherapies.
Casali’s team continually injected immunodeficient mice with human stem cells, which conditioned the mice to produce large amounts of estradiol. Previous work from Casali showed that the estradiol improves survival of human stem cells. The grafting of stem cells with estrogen conditioning allowed for the growth and differentiation of immune cells. The mice eventually reconstituted a human lymphoid and myeloid immune system. Consequently, this immune system was able to respond to infections and vaccinations. Complete humanized mice allow basic science to be more translatable now that scientists can test therapeutics and better understand how patients would respond. This also has the potential to eliminate the use of non-human primates for therapeutic and pharmacological studies. Now with a complete humanized model, physicians and scientists can better understand disease and provide more accurate treatments for patients.
Article, Nature Immunology, Paolo Casali, Long School of Medicine, UT Health San Antonio