New Approach Found to Reduce Toxicity in Immunotherapy
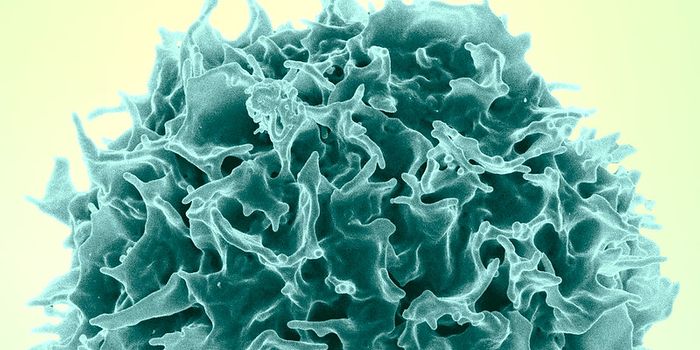
There are various ways to treat cancer. The gold standard has been chemotherapy for over 50-years. However, treatment with immunotherapy is quickly becoming commonplace in clinics. Immunotherapy is a different approach to treat diseases such as cancer and autoimmune disorders. This treatment focuses on redirecting the immune system to recognize and target foreign pathogens. In many cases, the tumor goes unnoticed by various immune cells and continues to proliferate. Immunotherapy aids in activating these immune cells to target the infectious disease. Immunotherapy can target a myriad of immune cells, but T cells are the primary target. T cells are critical cells in the body responsible for recognizing and killing or lysing infections. Different checkpoint inhibitors that block cell-to-cell interactions focus on T-cells. The cell-to-cell blockade results in T cells responding to foreign material and lysing the tumor.
Another form of immunotherapy is known as chimeric antigen receptor (CAR) T cell therapy. This form of treatment engineers T cells from a patient’s body to recognize markers on the tumor. The idea is to generate a stronger immune response toward the tumor once the T cells are programmed. The T cells are then reinfused in the patient. This work has quickly become a hot topic in the field of tumor immunology accompanied by significant improvement in the treatment of cancer. However, CAR T-cell therapy is limited to hematologic malignancies and is associated with high toxicities in patients. Currently, researchers are working to not only improve patient survival, but provide higher quality of life through reduced toxic side effects.
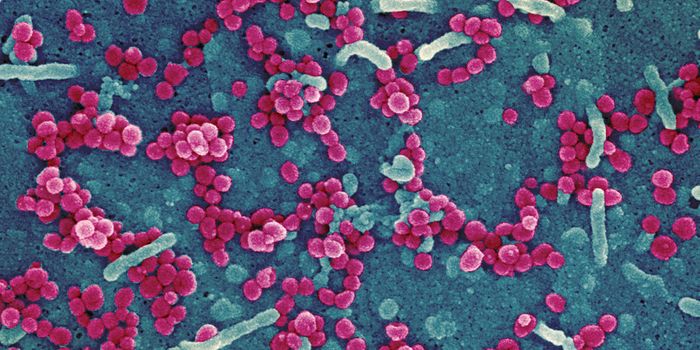
A recent article published in Cell Reports Medicine, by a group led by Dr. Markus Chmielewski, reported a way to make CAR T-cell therapy more effective with less toxic side effects. Chmielewski and his team analyzed lymphoma patient tissue samples from the University Hospital Cologne. The team found an increase in tumor surface markers: CD80 and CD86. Interestingly, these markers are restricted to tumor cells and cannot be found on other cells such as healthy B cells, which are the main cell affected in lymphomas. Therefore, the researchers used two different CAR designs or constructs to target B cell lymphoma and activate T cells.
Combining patient sample analysis and mouse models to test and confirm the mechanism of action, the team generated CAR constructs that targeted malignant cells only. One target includes CD19, which targets all B cells, and the others include CD80/CD86 due to their increased expression on malignant cells. In these therapies the CAR construct can recognize and bind to CD19 and CD80/86 to lyse the cell. This therapy will target the cells with all three surface markers and leave the CD19 positive healthy B cells alone.
The design of these CAR T-cell constructs increases specificity and reduces toxicity. Concurrently, the localized treatment only targets malignant B cells in lymphoma and maintains healthy B cell levels. The non-specificity of previous CAR constructs resulted in healthy cells being lysed increasing toxicity. Overall, Chmielewski and others found a novel strategy to improve CAR T-cell therapy in lymphoma patients. The new CAR T-cell construct is an optimal alternative to current CAR T-cell therapies by effectively lysing malignant cells and reducing toxicity in patients.
Article, Cell Reports Medicine, Markus Chmielewski, University Hospital Cologne