Novel Treatment Provides Less Invasive Approach for Diabetes
Over half a billion people in the world are living with diabetes. This disease is the result of low insulin levels in the body. Insulin helps break down sugar or glucose for cells to absorb and use for nutrients. If insulin is absent or low, less glucose is broken down for cell use. As a result, cells are deprived of nutrients and cannot function properly. If the disease is not treated, cells can rapidly die and cause serious injury to the patient. Unfortunately, there is no cure for diabetes. Currently, the best form of treatment is the administration of insulin through a pump or injection. In addition to the extra insulin, patients are recommended to go on a diet that is rich in nutrients, but low in fat and calories.
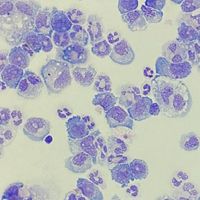
There are two subtypes of diabetes which describe why the body is not making enough insulin. The nomenclature describes these two subtypes simply as type 1 and type 2 diabetes. Type 1 diabetes is when the pancreas cannot make insulin due to the body’s immune system attacking the islet cells that make insulin. Type 1 diabetes usually appears in children and is a chronic autoimmune condition. Type 2 diabetes occurs when the pancreas produces lower levels of insulin, and the body eventually becomes resistant to the hormone. In both subtypes symptoms include extreme thirst, blurred vision, frequent urination, hunger, and fatigue. Since treatment for both types of diabetes are limited, many scientists are investigating how to better improve insulin delivery to enhance the quality of life in patients.
A recent article in Nature Biomedical Engineering, authored by two collaborating labs at Cornell University and University of Alberta, Edmonton demonstrated a novel technique to overcome autoimmunity in type 1 diabetes. The technique involves a device that is implanted under the skin of a patient which delivers insulin adequately and avoids immunosuppression. Dr. Minglin Ma at Cornell University and Dr. James Shapiro at the University of Alberta, Edmonton developed this technique to administer insulin less invasively and avoid immunosuppression implants.
The new technique is called Subcutaneous Host-Enabled Alginate Thread (SHEATH). The system delivers islet cells under the skin which produce insulin for the patient. SHEATH is a two-step process in which catheters are inserted under the skin for 4-6 weeks to allow blood vessels to form around them. The catheters are then removed, and the islet devices are then inserted into the space that the catheters created. The blood vessels remain intact and protect the inserted islet devices. This innovative technique allows for easy implant of islet cells and eliminates the discomfort from a pump or other more invasive treatments.
Ma, Shapiro, and others have found a novel way to better administer islet cells and increase insulin within the body. The benefit of this system is that you can complete it in an outpatient location, and it provides islets to the patient without the need for other treatments. However, long-term function of these islet devices still needs to be optimized. Islets under the skin is a revolutionary idea that has the potential to improve patient quality of life and provide long-term treatment for patients with type 1 diabetes.
Article, Nature Biomedical Engineering, Cornell University, University of Alberta, Edmonton, Minglin Ma, James Shapiro