Microbe That Causes Sepsis & Meningitis Has Mutated into a New Sexually Transmitted Disease
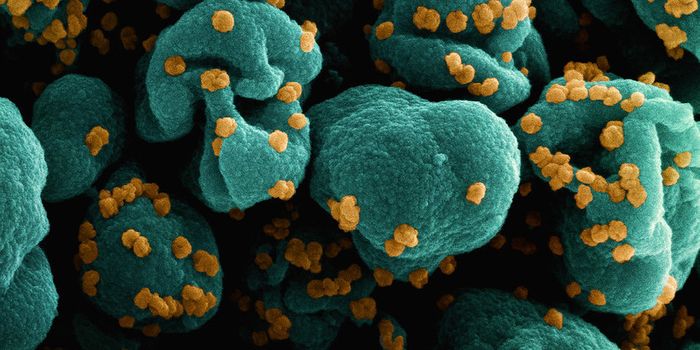
The ability of one microbe to adapt is giving it a whole new career as a sexually transmitted disease. Usually content with the back of the throat and nose of those who carry it, the dangerous pathogen Neisseria meningitidis has adapted to cause an illness that looks a lot like gonorrhea.
In 2015, a health clinic in Columbus, Ohio, experienced an upswing in the number of heterosexual men seeking treatment for urethritis, an inflammation of the urethra that causes painful urination. Initially thought to be due to infection with Neisseria gonorrhoeae, the bacteria that causes gonorrhea, doctors eventually determined they saw a sexually transmitted disease caused by N. meningitidis, instead. Since then, authorities have confirmed more than 100 cases in Columbus, with new cases reported in Indiana, Georgia, and Michigan.
Although closely related, N. gonorrhoeae and N. meningitidis typically live in and infect different environments. N. meningitidis usually resides in the respiratory system, while N. gonorrhoeae colonizes the urogenital tract, including the rectum, urethra, cervix, and vagina.
N. meningitidis is best known for causing meningococcal disease, a dangerous infection of the lining of the spinal cord and brain. The pathogen also causes an acute, often fatal infection of the bloodstream called sepsis. Transmitted through close contact, sharing utensils, or saliva, the invasive meningococcal disease at onset feels like a case of influenza but is accompanied by symptoms like a headache, stiff neck, or fever.
Before the development of a vaccine, between 800 and 1,200 cases of meningococcal disease were reported each year. Since then, between 600 and 1,000 people contract the disease, and approximately 10% to 15% of these victims die each year. About one in five of those who survive suffer permanent disability like organ or brain damage, loss of limbs, and other serious complications.
After conducting a genome analysis, scientists from the Emory University School of Medicine determined bacterial samples of N. meningitidis isolated in patients in the US leave a unique "molecular footprint" indicating the bacterium has structurally adapted to the urogenital environment as an STD.

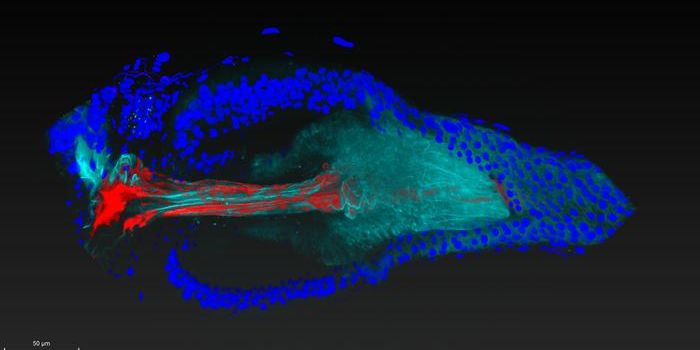
Stained N. meningitidis in spinal fluid.Image by Dr. M.S. Mitchell/CDC
Published in the Proceedings of the National Academy of Sciences, the study illustrates the swift adaptation of this bacteria to expand its residence from the respiratory to the reproductive system.
While N. meningitidis does not typically cause urogenital disease, there have been outbreaks of invasive meningococcal disease in urban areas like Paris, Berlin, and Los Angeles. Linked to populations of men who have sex with men, the route of transmission for these outbreaks was believed to be through oral and anal sex. Still, the authors report this is not the form of the bacterium that is emerging as an STD in regions throughout the US.
Instead, researchers identified a new clade of N. meningitidis that is adapted to the environment of the urogenital area, rather than the respiratory system. A clade is a group of organisms that evolves from a common ancestor.
Through whole genome sequencing, the infections treated in Columbus, Ohio, were found to be a "nongroupable" form of N. meningitidis instead of N. gonorrhoeae. This study took a close look at the microbe subtype to identify its genetic properties:
- This form of N. meningitidis appears to have acquired genes from N. gonorrhoeae that allow the bacterium to thrive in the low-oxygen environment of the urogenital region. The swapping of gene material suggests the two bacteria shared a common human residence.
- While N. meningitidis is encased in a protective capsule, this novel form of the bacterium, called US-NmUC, no longer has a capsule. Researchers suggest the loss of its outer structure gives the bacteria the capability to adhere to surfaces of mucous. Dropping the capsule also restructures the bacterium in a way that makes it less likely to cause invasive meningitis.
- Study authors suggest N. gonorrhoeae and N. meningitidis each adapted to a different environment. With the new form of N. meningitidis, the bacterium has borrowed some tools from gonorrhea to "better assimilate into the same niche first adopted by gonococci."
The good news is doctors effectively treated these patients with the novel clade with drugs used to treat gonorrhea. The bad news is that N. gonorrhoeae is known for its adaptability and growing resistance to drugs of choice used to treat it. There remains only one front-line group of medications to treat gonorrhea — the cephalosporins.
In a press release, lead author Yih-Ling Tzeng, assistant professor of medicine at Emory University School of Medicine, notes:
[A]s the gene conversion demonstrates, this clade can readily take up DNA from gonococci and it is not unthinkable that gonococcal antibiotic resistance genes could jump into this clade by gene transfer, if it is to its advantage.
It is not yet clear if vaccines developed against meningococcal disease could be effective against this new form of N. meningitidis. Without its protective capsule, proteins produced by the bacterium could be vulnerable to the vaccine. Because of its adaptability, and the tendency in some patients to contract repetitive infections, an effective vaccine for gonorrhea is not yet available.
The rate of sexually transmitted diseases in the US continues to rise. Anyone can get an STD, but certain groups, like young adults ages 15 through 24 and bisexual or gay men, have higher case counts. Both genders catch STDs, but the long-term consequences of an undiagnosed STD to a woman include infertility. According to the Centers for Disease Control and Prevention, STDs cause infertility in more than 20,000 women per year.
There is a new STD in town. If it gets cozy with N. gonorrhoeae and gene transfer occurs, drug resistance developed over time by gonorrhea could quickly become a feature of this novel pathogen. And remember, April is STD Awareness Month. Most people do not know they are infected until tested. Protect yourself and those you love, use a condom every time, and get tested.
This article was originally published on invisiverse.com