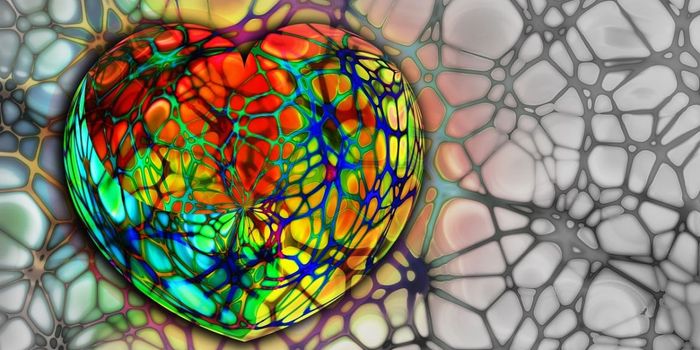
In this composite image, a human nerve cell derived from a patient with Rett syndrome shows significantly decreased levels of KCC2 compared to a control cell.
Image Credit: Gong Chen lab, Penn State University
Researchers found that a brain molecule KCC2 was lacking in nerve cells from Rett Syndrome patients. The discovery suggests a new approach to treating Rett by adjusting the brain molecule.
Rett Syndrome is a severe form of autism spectrum disorder that has no cure. The neurodevelopment disorder occurs almost only in girls. Rett patients experience language deficiencies, motor problems, seizures, balance issues, breathing problems, and other ill effects.
Infants with Rett experience a period of normal development for about 7 to 18 months. At the disease’s onset, the patient loses previously acquired skills, such as the ability to communicate. In this period of developmental regression, patients often exhibit autistic-like behaviors, seizures, and uncontrolled hand movements. The disorder’s progression and symptoms dramatically vary per person. Scientists do not fully understand the mechanism behind the delayed onset of the symptoms.
Rett is caused by mutations of the gene MECP2, which plays a critical role in the central nervous system. The gene is in every brain cell and located on the X chromosome.
Brain molecule KCC2 is an important downstream target of MECP2. This means the transcription of KCC2 may be dependent on McCP2. The lack of KCC2 results in a delayed GABA functional switch.
GABA neurotransmitters occur naturally in the brain and reduce the activity of the neurons it binds to. Without enough GABA, neurons would fire too often and cause symptoms such as anxiety.
"KCC2 controls the function of the neurotransmitter GABA at a critical time during early brain development," says Gong Chen professor of biology at Penn Sate. “When we put KCC2 back into Rett neurons, the GABA function returns to normal. [Thus,] increasing KCC2 function in individuals with Rett Syndrome may lead to a potential new treatment,” Chen said.
The most exciting part about the research is that it uses human neurons from Rett patients as a clinically relevant disease model, Chen said. "Therefore, the new drug target discovered in this study might have direct clinical implication in the treatment of Rett Syndrome and potentially for other autism-spectrum disorders as well.”
IGF1, which stands for insulin-like growth factor 1, is a molecule that was shown to reduce Rett symptoms in a mouse model. The researchers found that treating the diseased nerve cells with IGF1 raised the level of KCC2. The raised level fixed the function of the GABA neurotransmitters.
"The finding that IGF1 can rescue the impaired KCC2 level in Rett neurons is important not only because it provides an explanation for the action of IGF1, but also because it opens the possibility of finding more small molecules that can act on KCC2 to treat Rett Syndrome and other autism spectrum disorders," said Xin Tang, a graduate student in Chen's Lab and the first-listed author of the paper.
IGF1 is in an ongoing phase-2 clinical trial for the treatment of Rett in humans.
The paper was published on January 4, 2016, in the journal
Proceedings of the National Academy of Sciences Early Edition.
Sources:
“KCC2 rescues functional deficits in human neurons derived from patients with Rett syndrome” (full article) via
PNAS Early Edition,
Penn State press release,
National Organization for Rare Disorders (NORD),
Gizmag,
Scientific American