Almost 80,000 people die each year worldwide due to brain inflammation diseases, and it’s hard to know how many of these deaths could be prevented with better diagnoses. A new study from Johns Hopkins Medicine serves to make better diagnoses a reality by incorporating the latest advances in genetic sequencing of brain tissue.
Better diagnosis, better treatment plan. That’s what the scientists from Johns Hopkins were thinking when they launched their clinical study of 10 patients with clinical signs of a brain infection. Any fever or neurological symptoms were accepted, including limb weakness, partial paralysis, numbness, headache, or seizures. Six patients were male; four were female. Patients ranged in age between 16 and 68.
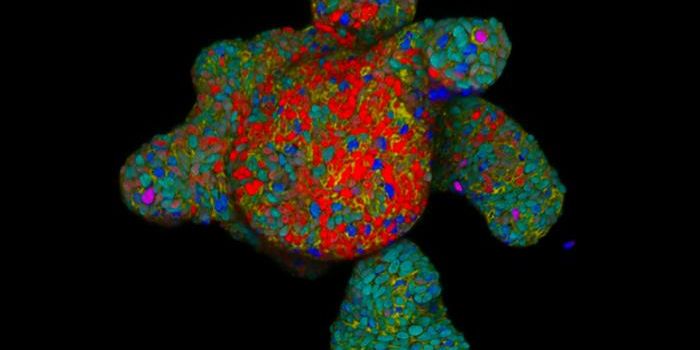
Researchers obtained tissue samples from the patients’ brain lesions, the location of damaged tissue where the infection was the worst. They knew the location thanks to images from magnetic resonance imaging (MRI) results. The genetic sequencing technology used to analyze the tissue samples can read millions of DNA strands at once, and upon receiving the information, the researchers were then able to compare the results with a database packed with genetic information from human and nonhuman DNA sequences, bacterial genomes, viral genomes, and single-cell pathogen genomes.
Not counting the matches with human DNA, the researchers made a “top three” list for each patient per the potentially infectious organisms whose DNA they found in their brain tissue.
Diagnosis Successes
For three patients, the sequencing results precisely pinpointed the causative agent. The pathogens to blame were
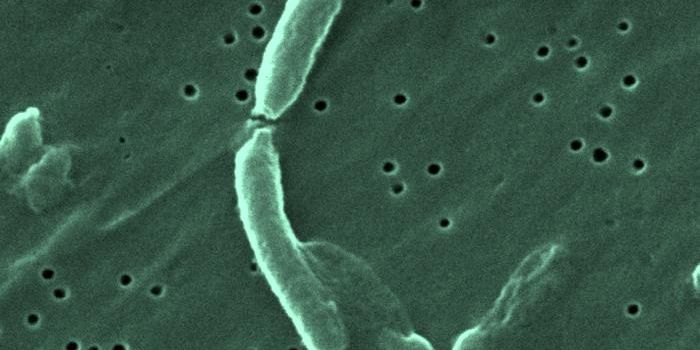
Mycobacterium tuberculosis, JC virus, and Epstein-Barr virus.
M. tuberculosis, the bacteria species that is responsible for tuberculosis, also causes a rare type of meningitis, the name for an infection of the brain and spinal cord. It is actually not uncommon to be positive for JC virus; a study in 2006 showed 40 to 60 percent of the world’s population has the virus by the time they reach ten years of age. However, for people with weakened immune systems, the virus can travel to the brain and cause progressive multifocal leukoencephalopathy, a disease that affects myelin, which neurons rely on for insulation. Lastly, Epstein-Barr virus, most known for causing mononucleosis in humans, can also cause viral meningitis and encephalitis.
With three causative agents nailed down, doctors could continue with treatment for these patients specific to their need, but what about the other seven patients?
Inconclusive but still helpful
For two of the remaining patients, the study results were slightly inconclusive. One of the two appeared to have multiple types of a bacteria called
Delftia acidovorans, which was easily treated with antibiotics. The other patient seemed to have many types of
Lactococcus bacterial species. However, the researchers actually discovered a year later after reanalyzing the data with an updated database that the pathogen causing brain disease was actually called
Elizabethkingia, a bacterial species discovered so recently that its genome had not been added to the database during the initial study. Scientists now know that
Elizabethkingia is found in soil and can cause meningitis.
The five other patients were not as lucky to receive such decisive answers from the genetic sequencing test. Whether the genome of the pathogen causing their infection has not yet been accounted for or the pathogen was simply able to hide undetected from genetic screening, a solution for their infection has yet to be found. However, scientists did know what was
not causing their infection, and they could avoid giving treatment that they knew was irrelevant.
Limitations
Like the patient who ended up having an
Elizabethkingia infection, future use of genetic screening to diagnose brain infections is only as helpful as the breadth of the database to which researchers can compare their results. However, as research continues and databases grow, using genetic sequencing as a diagnosis tool will become more useful. Additionally, more research into the healthy populations of bacteria that may reside in the brain, like the healthy gut bacteria that help with digestion, is important for picking out which bacteria are normal and which should be removed. “Having a correct diagnosis is the only way to ensure the best, individualized precision treatment,” said Carlos Pardo-Villamizar, MD.
The next step to make the dream of using genetic sequencing for diagnosing brain infections a reality is to complete “validation studies” incorporating patients with “already established” diagnoses. By running genetic sequencing tests on these patients and following the same steps of comparison to the existing database, researchers will be able to know more about the rate of false-positive and false-negative results. There’s much to be done, and researchers are well on their way.
This study was recently published in the journal
Neurology: Neuroimmunology and Neuroinflammation.
Sources:
Johns Hopkins Medicine,
Institute for Health Metrics and Evaluation,
MedlinePlus,
Clinical Infectious Diseases, National Institute of Neurological Disorders and Stroke,
Centers for Disease Control and Prevention