IBS and Depression Have Genetic Risk Factors in Common
Irritable bowel syndrome (IBS) is a common condition around the world, and it can cause bloating, abdominal pain, and dysfunction that significantly impacts some people's quality of life. (It is not the same as inflammatory bowel disease, an umbrella term that can refer to Crohn's disease and bowel cancer). Mood and anxiety disorders are also common everywhere. Scientists have now found that some genetic risk factors are shared by IBS and psychiatric disorders. This research can give scientists a better understanding of the biological basis of these issues, which may open up new treatment options.
Reporting in Nature Genetics, researchers analyzed genetic data from over 40,000 people in the UK Biobank who were diagnosed with IBS, and 12,852 participants in a global study searching for IBS-linked genes. That data was compared to genetic information from 433,201 individuals that did not have IBS. Another analysis was performed using genetic data from 23andMe Inc. customers who consented to being a part of research studies; this assessment included 205,252 individuals with IBS and 1,384,055 people without IBS.
The study indicated that IBS is generally not a condition that we inherit or get from our genes. Environmental conditions seem to have a far greater influence on the likelihood that a person will develop IBS, and that when many family members have IBS, it may be due to shared behavioral patterns, diets, or stresses.
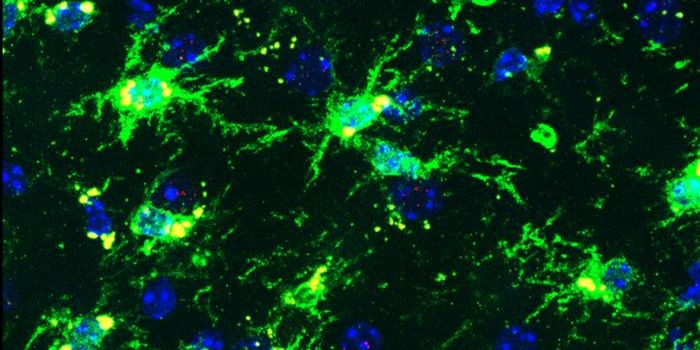
Some genetic factors did emerge, however. Six genes carried variants that were more common in people with IBS compared to controls: NCAM1, CADM2, PHF2/FAM120A, DOCK9, CKAP2/TPTE2P3 and BAG6. But these genes, surprisingly, are not active in the gut. Instead, many have roles in the brain and potentially, nerves that signal to the gut.
A pattern emerged in which the genetic susceptibility for IBS was overlapping with vulnerability to mental health conditions; some of the same genetic factors that raise a person's risk of IBS also seem to increase the risk of anxiety and mood disorders, including depression, anxiety, and insomnia. This evidence does not indicate that there is a causal relationship, noted the researchers; this should not be interpreted that IBS causes anxiety or vice versa.
"IBS is a common problem, and its symptoms are real and debilitating. Although IBS occurs more frequently in those who are prone to anxiety, we don't believe that one causes the other. Our study shows these conditions have shared genetic origins, with the affected genes possibly leading to physical changes in brain or nerve cells that in turn cause symptoms in the brain and symptoms in the gut," explained co-senior study investigator Professor Miles Parkes of the University of Cambridge.
This research also suggested that when someone has had both anxiety and IBS, they were more likely to have received frequent antibiotic treatments in childhood. Antibiotics are known to disrupt the gut microbiome, which has a close link to human health.
While genes may only be having a small influence on IBS, even a subtle impact could provide scientists with the information they need to identify the pathways that should be targeted for treatment, noted lead study author Chris Eijsbouts of the University of Oxford. Large human studies like this one can reveal those subtle patterns.
Sources: University of Cambridge, Nature Genetics