Using Wastewater to Identify COVID-19 Hotspots
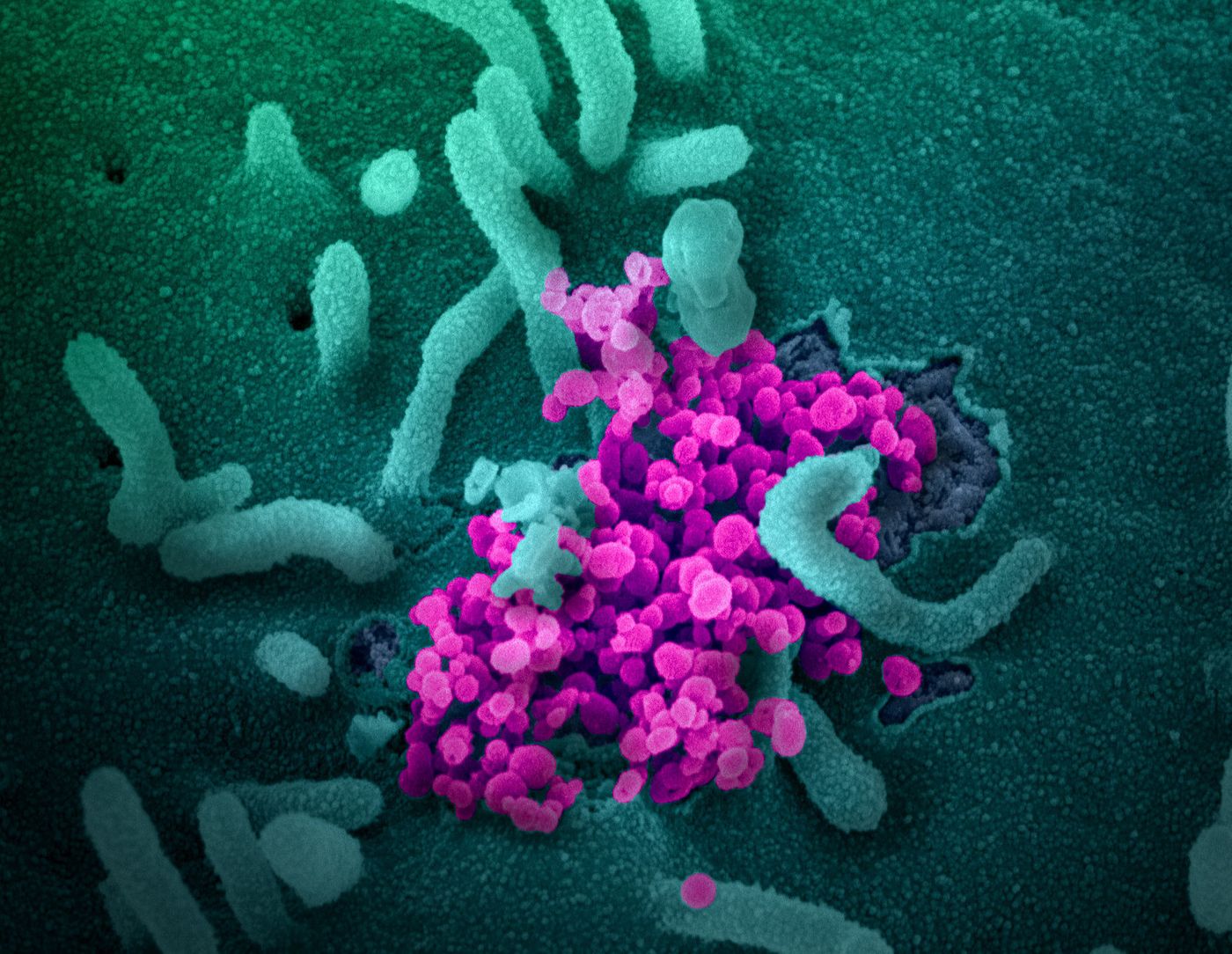
The SARS-CoV-2 pandemic is now known to have infected over 2.7 million individuals and killed at least 194,000. We are still learning about this virus, which only emerged in the past few months. But, we know that it's highly contagious and that it has probably infected many more people than we're aware of.
Infectious diseases can be managed if infected individuals can be identified with tests, and their contacts can be isolated, which reduces the spread of the disease. But testing has been a problem for the United States since the start of the pandemic, and the nation is still having trouble managing the scale and scope of the response. It may now be necessary to apply new tools to find virus hotspots.
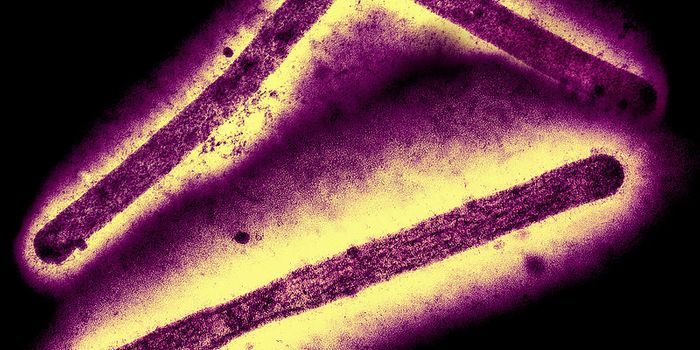
One of those tools is wastewater-based epidemiology (WBE), which analyses sewage to get information about the health of a community. Arizona State University (ASU) scientists have now reported in Science of the Total Environment that this method can be used to learn more about local and national COVID-19 levels.
"Our results show that exclusive reliance on testing of individuals is too slow, cost-prohibitive, and in most places, impractical, given our current testing capacity," said Rolf Halden, director of the Biodesign Center for Health Engineering at ASU. "However, when preceded by population-wide screening of wastewater, the task becomes less daunting and more manageable."
This tool may also be especially for impoverished areas and other nations where the healthcare infrastructure is likely to be overwhelmed by a COVID-19 outbreak; it can help identify a potential hotspot before it gets out of control. The US has the largest WBE network, and SARS-CoV-2 indicators have been added to the list of health markers it tracks.
The technique created by Halden's team can indicate the presence of a single infected person from a pool of 100 to two million people. The tool uses a common molecular method called real-time quantitative reverse-transcriptase PCR (qRT-PCR) to amplify fragments of the SARS-CoV-2 genome that are present in a sample.
"We can in one go monitor an entire community for presence of the new coronavirus," Hart said. "However, tradeoffs exist. To get the best results and avoid loss of information, we want to measure close to virus hotspots and take into account wastewater temperature and dilution when estimating the number of infected cases."
Under the best-case scenario, hardly anyone would be infected, but if one person in a community of two million had the virus, we would know. When infection rates are much higher, the test can determine if there is one infected person in a community of 114. This tool could help show where hotspots exist, and efforts to reduce transmission like social distancing could then be applied in a more specific way.
Halden suggested that this tool could be used to screen about 70 percent of the US population using 15,014 wastewater treatment plants at a cost of around $225,000. This approach would enable us to find out where the virus was having the greatest impact, and a more targeted system could be put in place to screen individuals for infection.
Sources: AAAS/Eurekalert! via Arizona State University, Science of the Total Environment