Researchers Reveal New Details About How SARS-CoV-2 Infects Cells
While studies have shown that the SARS-CoV-2 virus, which causes COVID-19, enters cells through a receptor called ACE2 (and potentially other receptors such as TMPRSS2), research has now revealed new details about how infection occurs. The epithelial tissue lining the nasal cavity is mostly made up of a few cell types, one of which are multiciliated cells; they form a protective barrier that keeps invaders from getting into the airways. The researchers used an organoid model of the human upper airway to show that SARS-CoV-2 only infected ciliated cells. Once those cells were infected, the virus seems to use mucus to spread further, into other cells. The findings have been reported in Cell.
The multiciliated cells in nasal epithelium carry structures called microvilli, spikes that protrude from cells and move particles. One multiciliated cell can also have hundreds of motile cilia, and they beat in sync. (Motile cilia are different from primary cilia, sensory organelles that act like little antennae on many cell types.) Motile cilia move mucus and a protein called mucin, around the nasal cavity. Mucus is critical for keeping cells moist, and trapping debris and pathogens.
Mucin molecules can link together to generate kind of three-dimensional, stretchy mesh. The epithelial motilr cilia push through this layer, beating to push mucus, and anything trapped in it to a place where it is sneezed or blown out, or swallowed and digested.
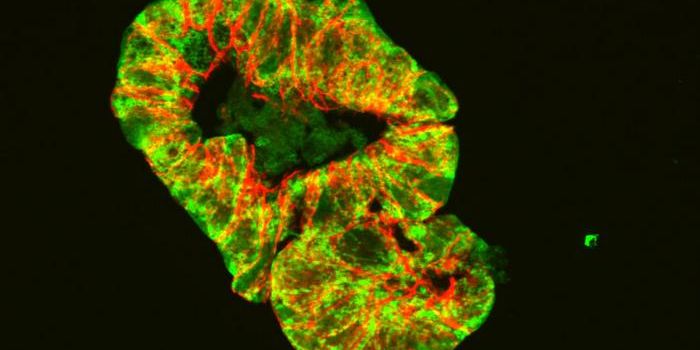
The airway epithelial organoids generated for this study did not have immune cells or blood vessels, but they mimicked the epithelial structure, the mucin layer, and contained multiciliated cells. The organoids were exposed to SARS-CoV-2, and the researchers observed the cultures with advanced microscopy and immunostaining.
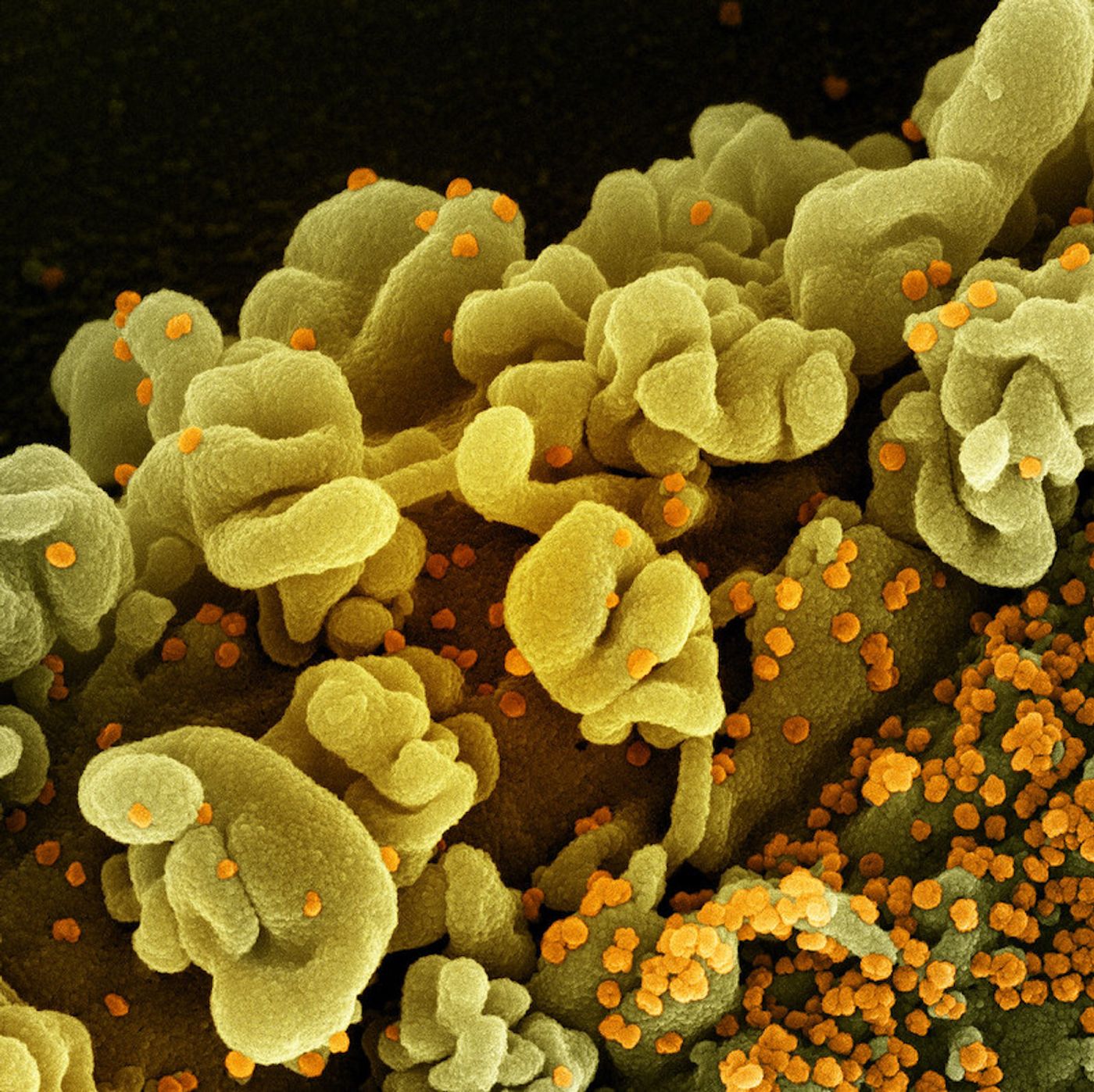
This revealed that only ciliated cells were infected with the virus, which exclusively attached to motile cilia at first. Six hours after the organoids were exposed to the virus, many viral particles covered the sides of the motile cilia. After 24 hours, the virus was only replicating a little, but at 48 hours, there were massive amounts of replication. This aligns with observations in animal models and people that the virus takes a day or two to start replicating.
When the researchers eliminated motile cilia from the organoids by removing a protein crucial for their formation, the viral infection was slowed significantly.
The upper airways are a "launchpad" the virus uses for infecting us and others, and "It's clear that human ciliated nasal epithelial cells are the primary entry site for SARS-CoV-2 in nasal epithelial tissue," said co-senior study author Peter Jackson, Ph.D., a Stanford Medicine professor of pathology and of microbiology and immunology.
The researchers also suspected that the mucus barrier was causing the infection delay. When the mucin network was broken, down, the virus entered the cells more easily.
The virus also uses microvilli. When the virus has infected multiciliated cells, it triggers enzymatic activity that causes microvilli to increase in number, get bigger, and form wild branches that punch through the mucus barrier. Viral particles attach to these branches, and from there, they can move along with the mucus to other types of cells in other parts of the body. When the investigators interfered with the enzymes that transformed microvilli, the virus was less able to infect other cells.
These results were confirmed with the BA.1 strain, a variant of SARS-CoV-2 Omicron, as well as respiratory syncytial virus and parainfluenza virus, suggesting that these observations may apply in a general way to many respiratory viruses. The study also confirms what other researchers have suggested - an intranasal spray could be very effective against COVID-19.
Sources: Stanford University, Cell