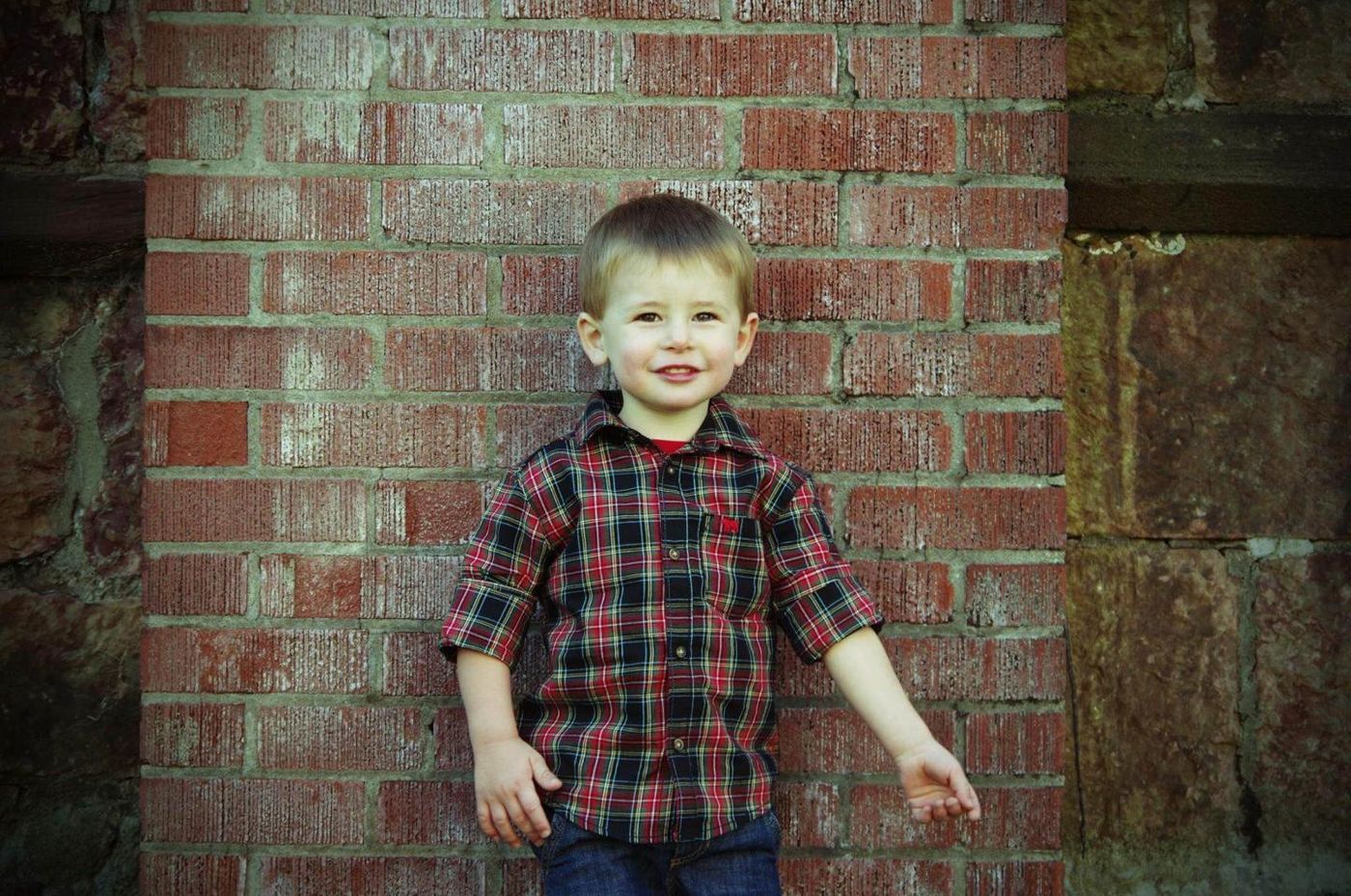
You wouldn’t know that a now-healthy three-year-old had prenatal heart surgery after just two months in his mother’s womb. Now the doctors who performed the surgery are calling the procedure an official success, and they published their findings in a new article in the
American Journal of Obstetrics and Gynecology.
"We have shown that we can accurately diagnose and provide a prognosis for this rare condition in utero, as well as perform fetal surgery," said co-study leader Jack Rychik, MD, director of the Fetal Heart Program at The Children's Hospital of Philadelphia (CHOP).
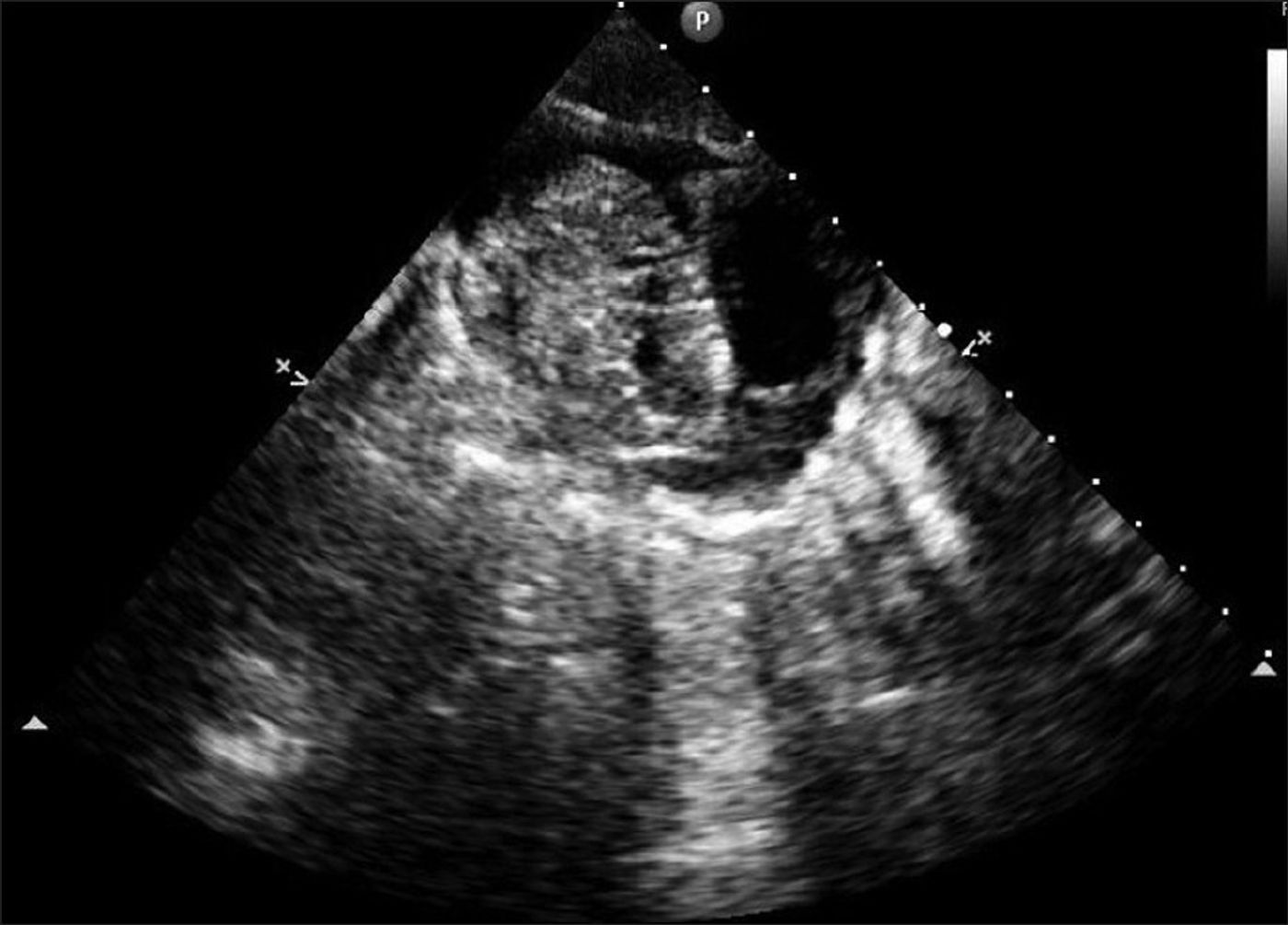
Intrapericardial teratomas are rare cardiac tumors that develop in the pericardium, the sac surrounding the heart, and grow quickly. They can be detected during the fetal period, but they are deadly if not treated and waiting until birth is often too late. Before scientists from CHOP started doing prenatal heart surgery, the procedure for fetuses with these tumors involved draining the pericardial fluid, but only to prevent fetal heart failure until the baby was ready for delivery.
Waiting to perform surgery until the baby is delivered poses a lot of risks. Despite draining, the tumor could grow quickly, causing fluid to build up around the heart, putting pressure on it. This disrupts normal fetal circulation, causing death. To avoid fetal death, the CHOP team conducted the prenatal heart surgery in the now healthy three-year-old, the first time the surgery produced a live, healthy child after birth.
“Survival with good outcome may be possible in some patients," said Rychik. "It was the ability to bring so many different disciplines to the table that made us confident enough to take the leap to offer in-utero surgery on a fetal heart as a viable option.”
Rychik and his team started with a case series of eight fetuses with potential intrapericardial teratomas. Two were found to have other types of heart-related tumors, and four out of the six confirmed to have intrapericardial teratomas were not healthy enough to benefit from surgery. Two fetuses did undergo surgery, and they both survived.
One baby underwent open-fetal surgery at 24-weeks gestation, while the other underwent a different procedure: ex utero intrapartum treatment (EXIT) at 31 weeks gestation. EXIT procedures involve surgeons partially delivering the baby through a small incision in the mother’s uterus, conducting the surgery while the fetus is still connected to the placenta.
While CHOP researchers are excited about the success of the two surgeries and hopeful for prenatal surgeries of all kinds in the future, there are certain inherent risks for both the baby and the mother that accompany these types of procedures. However, many technological advantages of present-day medicine make a successful surgery more likely: improved prenatal imaging and improved cardiovascular surveillance through fetal echocardiography.
Source:
Circulation,
The Children's Hospital of Philadelphia