Cancer's Trick to Thriving in Low Oxygen

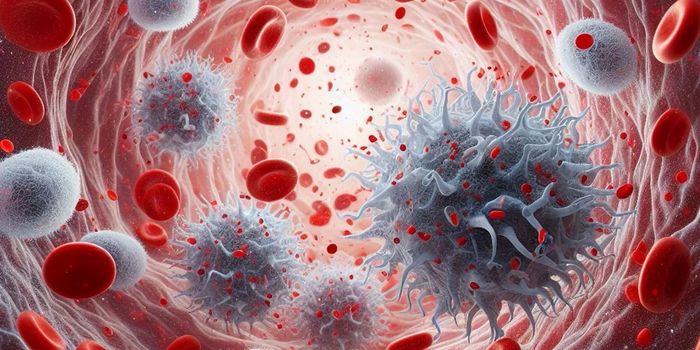
In cancer, scientists note a strange correlation: tumors that had low oxygen seemingly couldn’t cope and died off, but patients with these types of tumors fared the worst. A recent investigation by Johns Hopkins scientists shed light on this conundrum and could point to new therapeutic targets. As it turns out, cancer has a trick whereby it survives and thrives in low oxygen levels by adopting the same mechanisms used by embryonic stem cells.
Stem cells are those that have the capacity to divide indefinitely and differentiate into many types of cells in the body. These unique abilities are what make stem cells so attractive in regenerative medicine. But unfortunately, cancer cells have learned how to exploit this ability to enhance their own survival when oxygen is scarce.
Researchers have known that the oxygen content in tumors, particularly in breast tumor, is quite low at 1.4 percent, compared to the 9 percent in healthy tissues, and 21 percent in the atmosphere that we breathe. In these hypoxic (low oxygen) conditions, cells stimulate the increase of proteins known as HIFs (hypoxia-inducible factors), which then cause a cascade of other genes to be activated. The key gene from this cascade that’s used by cancer cells is NANOG, a quintessential pluripotency factor in stem cell reprogramming.
"Chemotherapy may kill more than 99 percent of the cancer cells in a tumor but fail to kill a small population of cancer stem cells that are responsible for subsequent cancer relapse and metastasis," said Gregg Semenza, the C. Michael Armstrong Professor of Medicine, a member of the Johns Hopkins Kimmel Cancer Center, and senior study author.
As such, the research team hypothesized that cancer cells in breast tumors survive in hypoxic conditions by using NANOG to revert to embryonic cell states. "The search has been intense to find these cells ‘Achilles heel.’ If we could get cancer stem cells to abandon their stem cell state, they would no longer have the power to keep repopulating tumors," Semenza added. Their suspicions about NANOG were confirmed, as they found that hypoxic conditions increased HIF proteins, which then led to increased NANOG mRNA transcript levels.
Cells quiet NANOG expression and suppress their pluripotency states by adding a chemical methyl tag on the gene’s mRNA transcript – a process known as methylation. If NANOG expression is lowered, cells could be forced to abandon their stem cell states and differentiate into other mature cells, potentially those more susceptible to low oxygen conditions.
To test this idea, the researchers honed in on another gene, ALKBH5, which acts to decrease methylation of NANOG transcripts, and thus increase NANOG expression. In cell experiments that block ALKBH5’s expression, the team found reduced NANOG levels due to methylation and a subsequent decrease in the number of cancer stem cells. Conversely, they reported increased NANOG levels and more breast cancer stem cells when ALKBH5 levels grew.
Taking their results to mice that were injected with 1,000 triple-negative breast cancer cells, the team noticed the same promising trend. That is, mice injected with cells missing ALKBH5 had reduced incidence of tumor growth; 43 percent of mice showed tumor growth. In contrast, all mice injected with unaltered breast cancer cells had tumor growth. "That confirmed for us that ALKBH5 helps preserve cancer stem cells and their tumor-forming abilities," said Semenza.
In the next phase, the research team plans to investigate whether the stem cell mechanisms also affect metastasis. They also aim to find other proteins involved in this pathway, which will perhaps point to new therapeutic avenues for breast cancer treatment. "There are still many questions left to answer but we now know that oxygen poor environments, like those often found in advanced human breast cancers serve as nurseries for the birth of cancer stem cells," said Semenza. "That gives us a few more possible targets for drugs that diminish their threat in human cancer."
Additional source: Hopkins Medicine press release