VISTA: A New Checkpoint for Cancer Immunotherapy
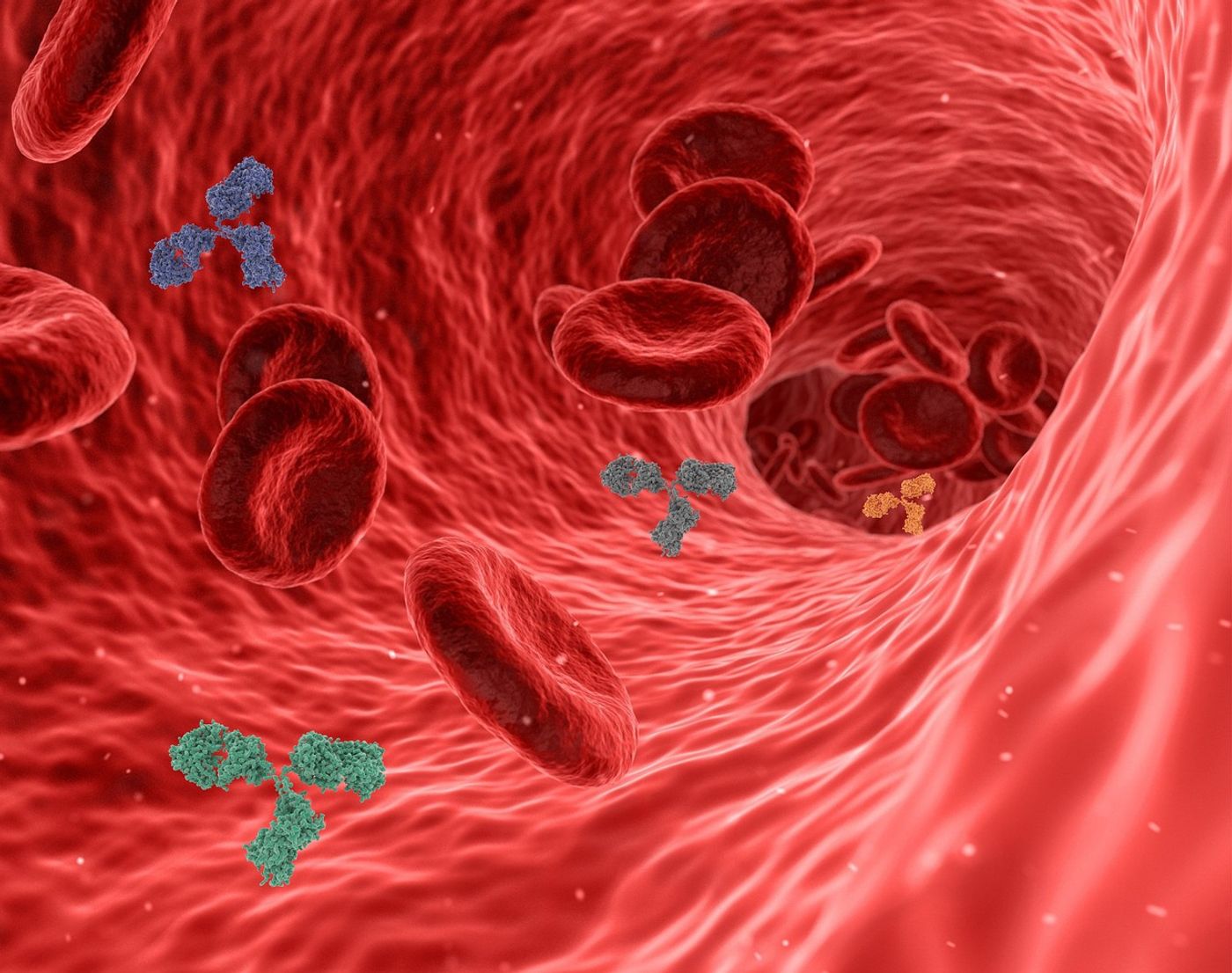
Over the past decade, immune checkpoint inhibitors (ICI) have revolutionized the cancer treatment area. These drugs block the interaction between proteins known as immune checkpoints and immune cells within our bodies. At times, immune checkpoints play a vital role in immune regulation, preventing unnecessary responses. However, tumors can upregulate proteins, thus evading an immune response, and in a tumor setting, this response is indeed necessary. ICIs interfere with checkpoint pathways and allow active immunity against cancer.
In 2011, the United States Foor and Drug Administration (FDA) approved the first ICI, ipilimumab, a CTLA-4 blocker, for treating advanced melanoma. Subsequently, ICIs targeting PD1 (pembrolizumab and nivolumab) and PDL1 (atezolizumab and durvalumab) received approval for treating various malignancies. Many clinical trials test the efficacy of novel ICIs in different settings.
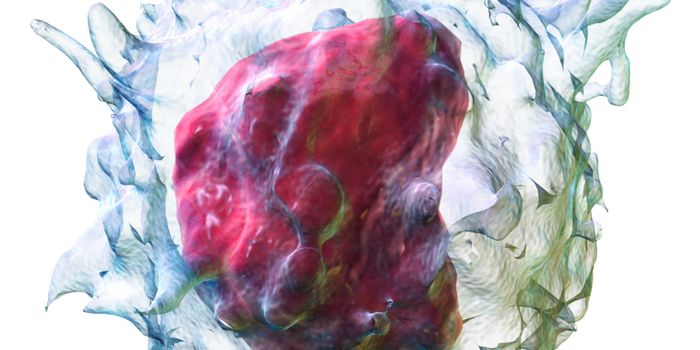
A recent study published in Science Immunology unveiled a promising new avenue for cancer immunotherapy and ICIs. The study evaluated a drug targeting an immune checkpoint molecule called VISTA (V-domain immunoglobulin suppressor of T cell activation), shedding light on its potential as an effective immunotherapy target.
VISTA, a key regulator of immune responses, has been found to be overexpressed in various cancers, leading to immune evasion. This study provides crucial insights into how targeting VISTA could enhance anti-tumor immune responses.
The researchers identified a marker called LRIG1 (leucine-rich repeats and immunoglobulin-like domains 1) as VISTA’s binding partner. When LFIG1 binds VISTA, an inhibitory response leads to suppression of T cells, vital immune cells needed for anti-tumor immune responses. This interaction between LRIG1 and VISTA acts as a brake on the immune system, preventing it from mounting a strong anti-tumor response. Inhibiting this interaction could release the brake and allow the immune system to attack the tumor more effectively.
The study used mice without LRIG1. These mice exhibited impressive anti-tumor immune responses. Specifically, mice lacking LRIG1 had increased numbers of tumor-specific T cells known as cytotoxic T lymphocytes (CTLs). Importantly, CTLs in the LRIG1 deficient mice were primed and ready to seek out and destroy cancer. In addition, the CTLs exhibited increased anti-tumor functionality and lived longer.
The findings on LRIG1 are of particular significance. They have measured LRIG1 expression on CTLs infiltrating the tumors of melanoma patients, unveiling a potential link between high LRIG1 expression and resistance to immunotherapy. This discovery could have a profound impact on future treatment strategies.
The study has demonstrated the feasibility of VISTA as an immune checkpoint molecule inhibited by LRIG1. Further research could potentially establish the VISTA/LRIG1 pathway as a highly effective target for immunotherapeutic approaches to cancer treatment.
Sources: Nature, BCJ, Sci Immunol