Olaparib, an experimental twice-daily oral cancer drug, produces an overall tumor response rate of 26 percent in several advanced cancers associated with BRCA1 and BRCA2 mutations, according to new research co-led by the Abramson Cancer Center of the University of Pennsylvania. The positive response provides new hope for patients with ovarian, breast, pancreatic and prostate cancers whose conditions have not responded to standard therapies. Results of the phase II study are available online in the current issue of the Journal of Clinical Oncology.
For the majority of patients in the study, olaparib was at least their third different cancer therapy. Based on the new data, the authors say olaparib warrants further investigation in phase III clinical trials. The positive response in metastatic pancreatic cancer patients who had received an average of two prior rounds of chemotherapy is an especially noteworthy finding, because the therapeutic options for these patients are limited.
The international research team studied nearly 300 patients with inherited BRCA1 and BRCA2 mutations who had advanced cancers that were still growing despite standard treatments. Patients were enrolled and treated at 13 centers around the world. In addition to the 26 overall shrinkage or disappearance rate in tumors following treatment with olaparib, researchers also found no further growth in cancer for at least eight weeks in 42 percent of patients. The overall survival at one year following treatment with olaparib was:
* 64 percent among ovarian cancer patients (with a median progression-free survival of 7 months)
* 45 percent among breast cancer patients (with a median progression-free survival of nearly 4 months)
* 41 percent among pancreatic cancer patients (with a median progression-free survival of nearly 5 months)
* 50 percent among prostate cancer patients (with a median progression-free survival of more than 7 months)
"By building on previous research, our study offers new hope for patients suffering from cancers caused by inherited BRCA1 and BRCA2 gene mutations," said Susan Domchek, MD, executive director of the Basser Research Center for BRCA at the University of Pennsylvania's Abramson Cancer Center, and senior author on the new study. "Olaparib was reasonably well tolerated in the current study, even in such a heavily pre-treated population, showing that PARP inhibitors such as olaparib potentially represent a much-needed advanced treatment option."
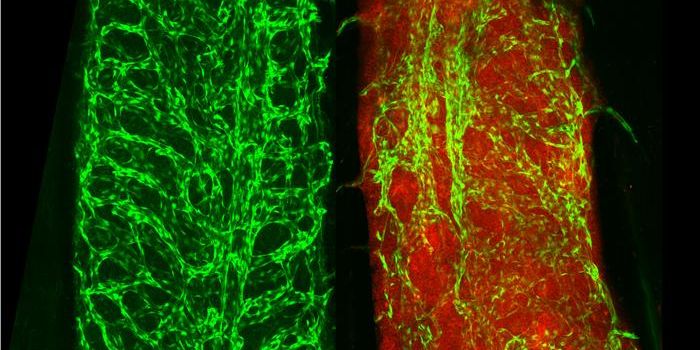
PARP - poly (ADP-ribose) polymerase - is used by healthy cells to repair themselves. Unfortunately, cancer cells also use PARP to repair DNA damage, thus extending their growth and possible lethality. Olaparib selectively binds to and inhibits PARP, potentially preventing it from repairing DNA damage in cancer cells, but not in normal cells. In cancers that also have a mutation in BRCA1 or BRCA2, this factor may help to control the tumor or shrink it.
BRCA1 and BRCA2 mutations in women increase the risk of several cancers, including breast and ovarian, while in males the BRCA2 mutation in particular has been tied to breast, prostate and pancreatic cancer. About five percent of breast cancers and ten percent of ovarian cancers are associated with an inherited mutation in BRCA1 or BRCA2.
Side effects were reported for 54 percent of participants, the most common of which was anemia (17 percent). Authors suggest the increased incidence of anemia compared to other studies may be due to the study population's longer history of cancer and higher number of prior chemotherapy treatments. Other side effects included fatigue, nausea and passing episodes of vomiting. Most toxicity could be managed by dose interruption and dose reduction.
The study was sponsored by AstraZeneca.
 Olaparib, an experimental twice-daily oral cancer drug, produces an overall tumor response rate of 26 percent in several advanced cancers associated with BRCA1 and BRCA2 mutations, according to new research co-led by the Abramson Cancer Center of the University of Pennsylvania. The positive response provides new hope for patients with ovarian, breast, pancreatic and prostate cancers whose conditions have not responded to standard therapies. Results of the phase II study are available online in the current issue of the Journal of Clinical Oncology.
Olaparib, an experimental twice-daily oral cancer drug, produces an overall tumor response rate of 26 percent in several advanced cancers associated with BRCA1 and BRCA2 mutations, according to new research co-led by the Abramson Cancer Center of the University of Pennsylvania. The positive response provides new hope for patients with ovarian, breast, pancreatic and prostate cancers whose conditions have not responded to standard therapies. Results of the phase II study are available online in the current issue of the Journal of Clinical Oncology.