Should cost be a concern in cancer testing? Female carriers of mutated BRCA genes have a significantly higher risk for developing breast and ovarian cancers than those who do not. Nonetheless, a new study by UCLA faculty questions the value of screening for the genetic mutations in the general population — including those who do not have cancer or have no family history of the disease — because of the high cost.
The UCLA researchers found that compared with universal screening, other diagnostic tools remain more efficient and might be more cost-effective. The study, authored by Dr. Patricia Ganz, director of the division of cancer prevention and control research at UCLA’s Jonsson Comprehensive Cancer Center, and Elisa Long, assistant professor at the UCLA Anderson School of Management, was published online by
JAMA Oncology.
According to the researchers, the BRCA genetic test that is most widely used today is too expensive to warrant universal screening, given how rare BRCA mutations are. They think the cost would need to drop by 90 percent for testing to be cost-effective for the whole population.
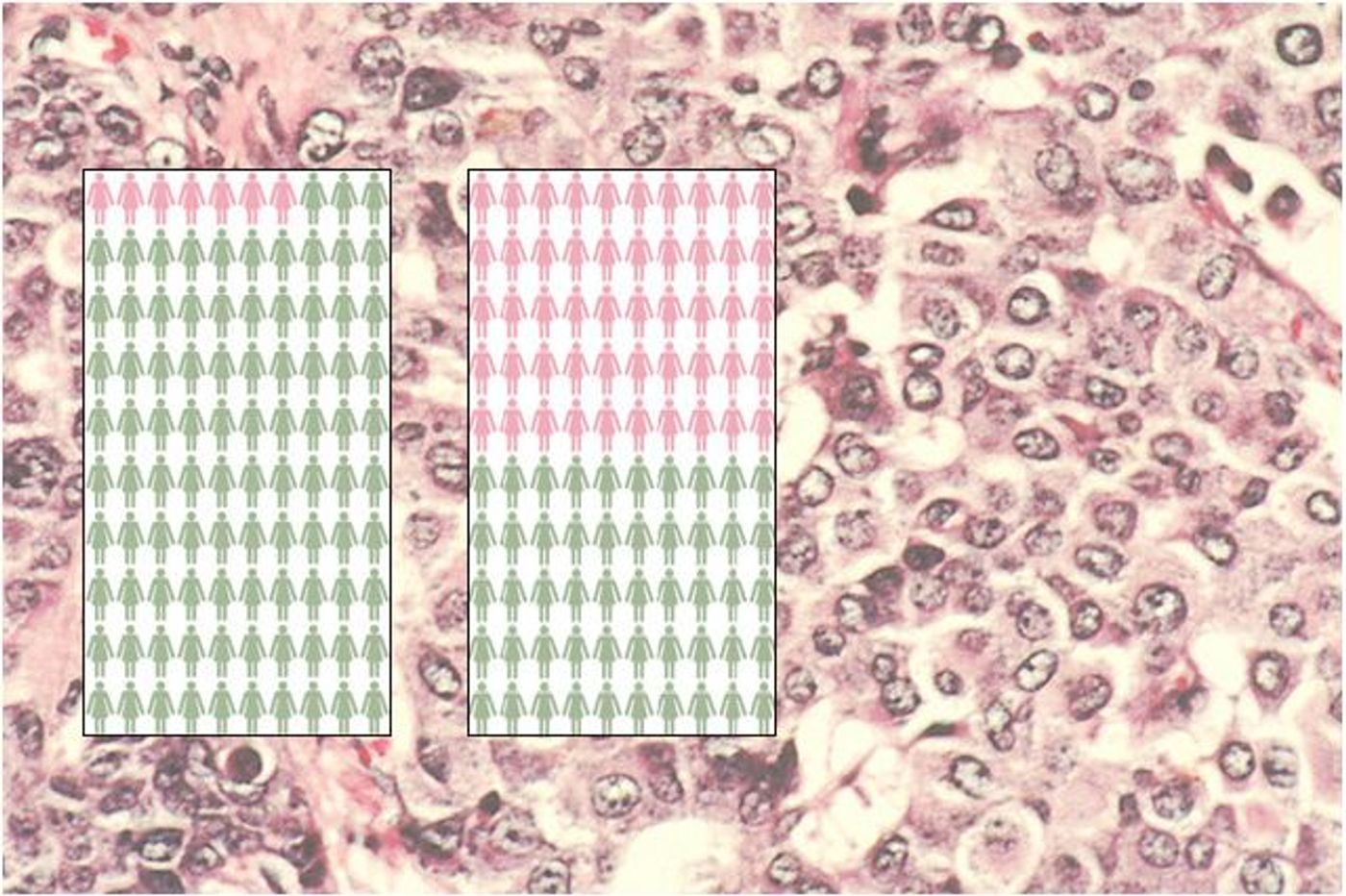
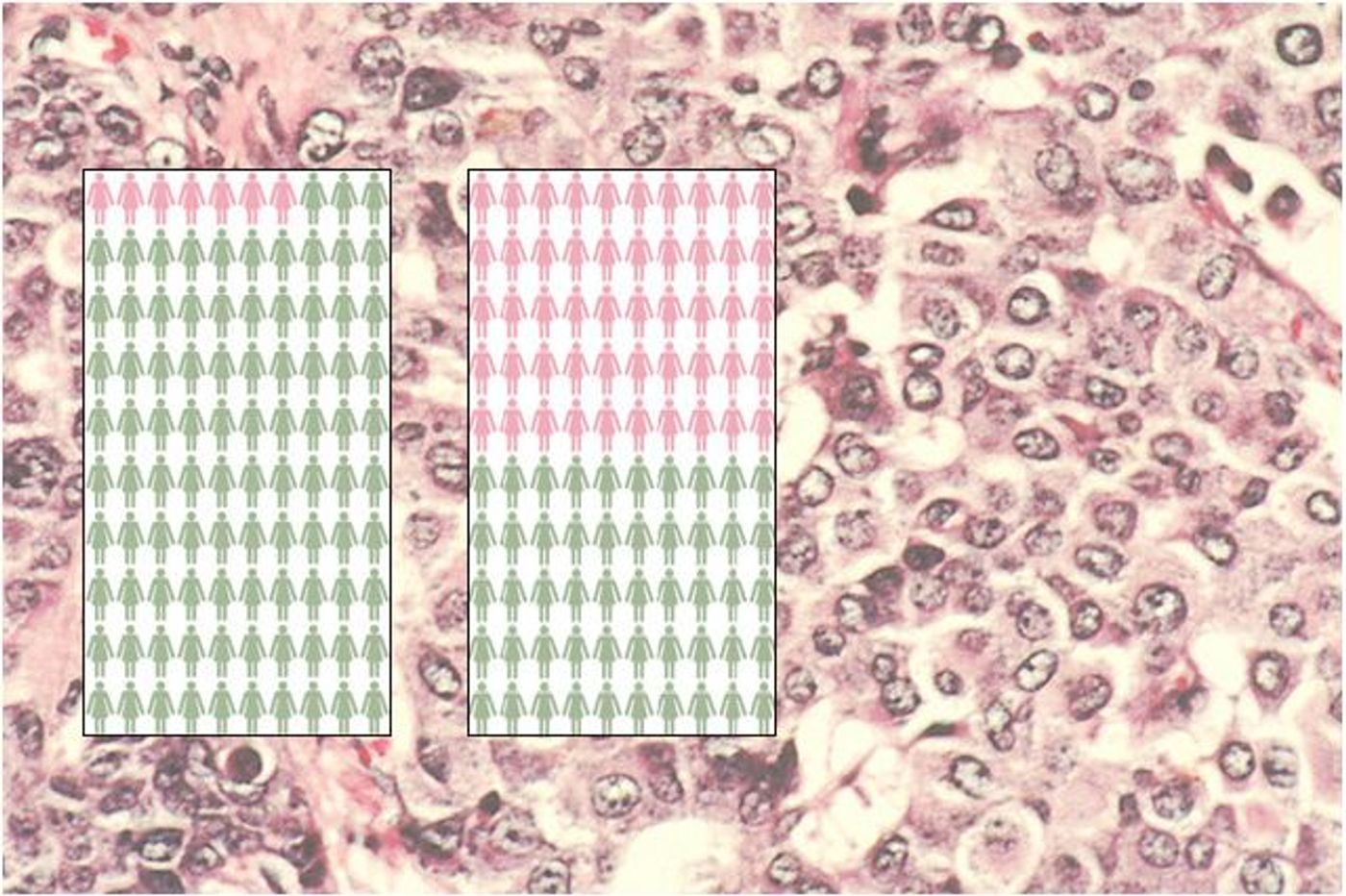
The researchers calculated that for every 10,000 women screened, BRCA screening could avoid four cases of breast cancer and two cases of ovarian cancer more than family history-based testing would and that BRCA screening would only extend patients’ life by an average of two days. They said that for 99.75 percent of women screened, a negative genetic test offers no increase in life expectancy.
The UCLA study adds to work by other researchers that analyzed genetic screening of women of Ashkenazi Jewish descent. In that population one out of every 50 women carries a harmful mutation. A larger percentage of this group could be identified as BRCA mutation carriers, so Long and Ganz found that the approach would yield an estimated 62 breast and 34 ovarian cancers avoided per 10,000 women tested, and gains in life expectancy that were 16 times higher than with universal screening. Of the 233,000 breast cancers diagnosed annually in the United States, only 5 to 10 percent can be linked to mutations in the BRCA genes. Women with breast cancer who carry these mutated genes usually develop the disease at a younger age, often in both breasts, and the cancer is often a more aggressive sub-type such as triple-negative breast cancer.
As Ganz and Long explained, harmful BRCA gene mutations are more likely to be found in families affected by breast and ovarian cancers. Carriers can pass the mutated genes to both daughters and sons. Those who carry a BRCA mutation are believed to have a 45 to 80 percent lifetime risk of developing breast cancer. Women carrying the BRCA-1 mutation have up to a 39 percent lifetime risk; women with BRCA-2 have a 10 to 17 percent lifetime risk for ovarian cancer. The U.S. Preventive Services Task Force advises BRCA genetic testing only for women with a known family history of breast, ovarian, tubal or peritoneal cancer.
Long, who had no family history of breast cancer, has a personal connection to the BRCA-1 mutation. She is a carrier, and last year, at just 33 years of age, she was diagnosed with triple-negative breast cancer, the most aggressive form of the disease. She was treated with six rounds of chemotherapy, a bilateral mastectomy and reconstructive breast surgery. The chemotherapy killed the cancer before her first surgery, increasing her five-year survival probability from 60 to 95 percent. She also had her ovaries and fallopian tubes removed, reducing her risk of ovarian cancer to less than 5 percent.
She concluded, “On a personal level, I would have benefited tremendously from universal BRCA testing, because I had no family history of breast cancer, but as a health services researcher I must also consider the relative value of different medical interventions. Many patients wish to know more about their genetic risk factors, and as more firms begin to offer genetic testing, we should expect the price to decrease, eventually making this an affordable policy.”