While mathematical models are powerful tools for demonstrating how cancer grows and spreads, they have an either/or problem, according to scientists at
Harvard University.
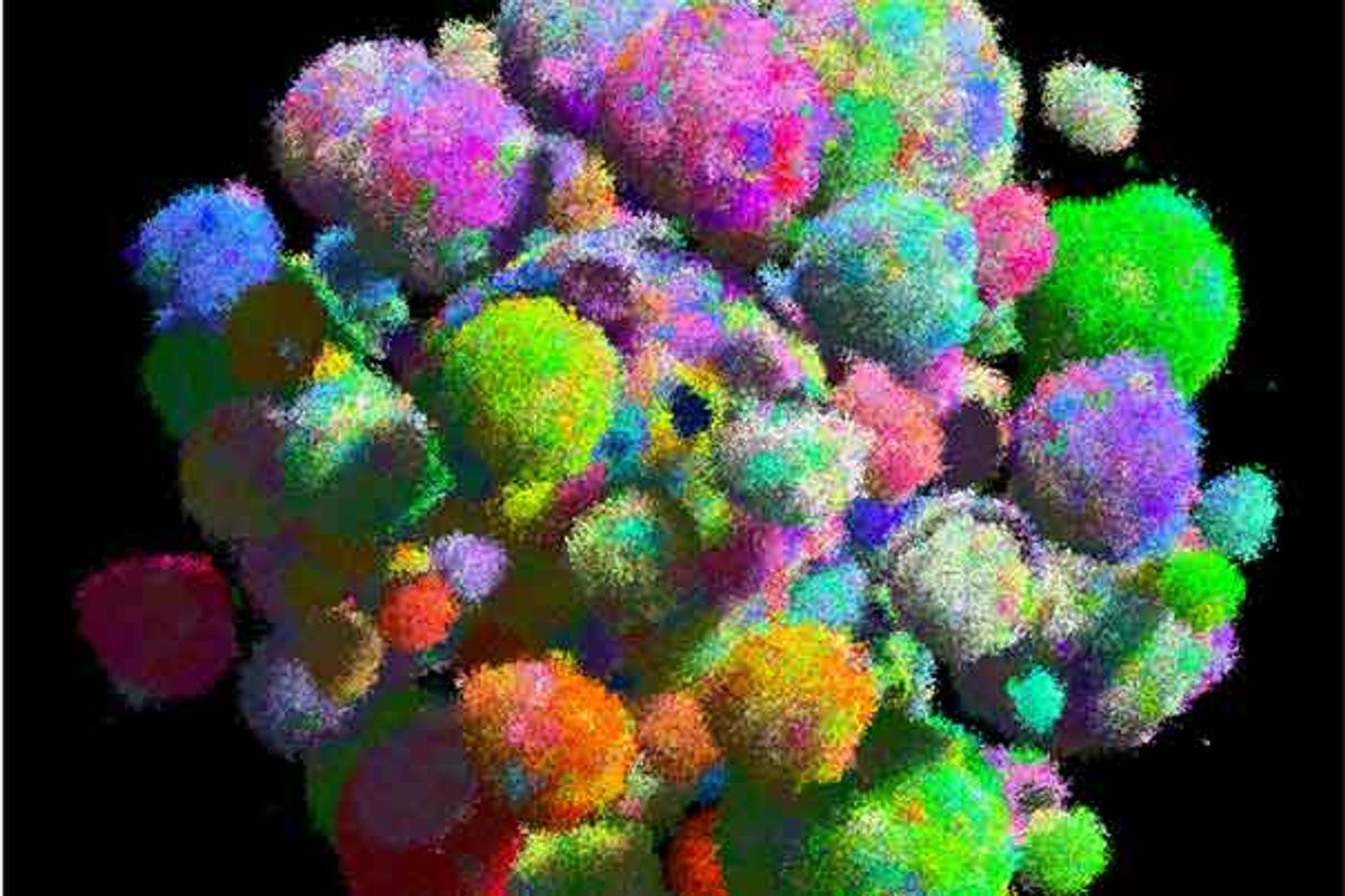
Harvard researchers combine mathematical and spatial models of cancer.
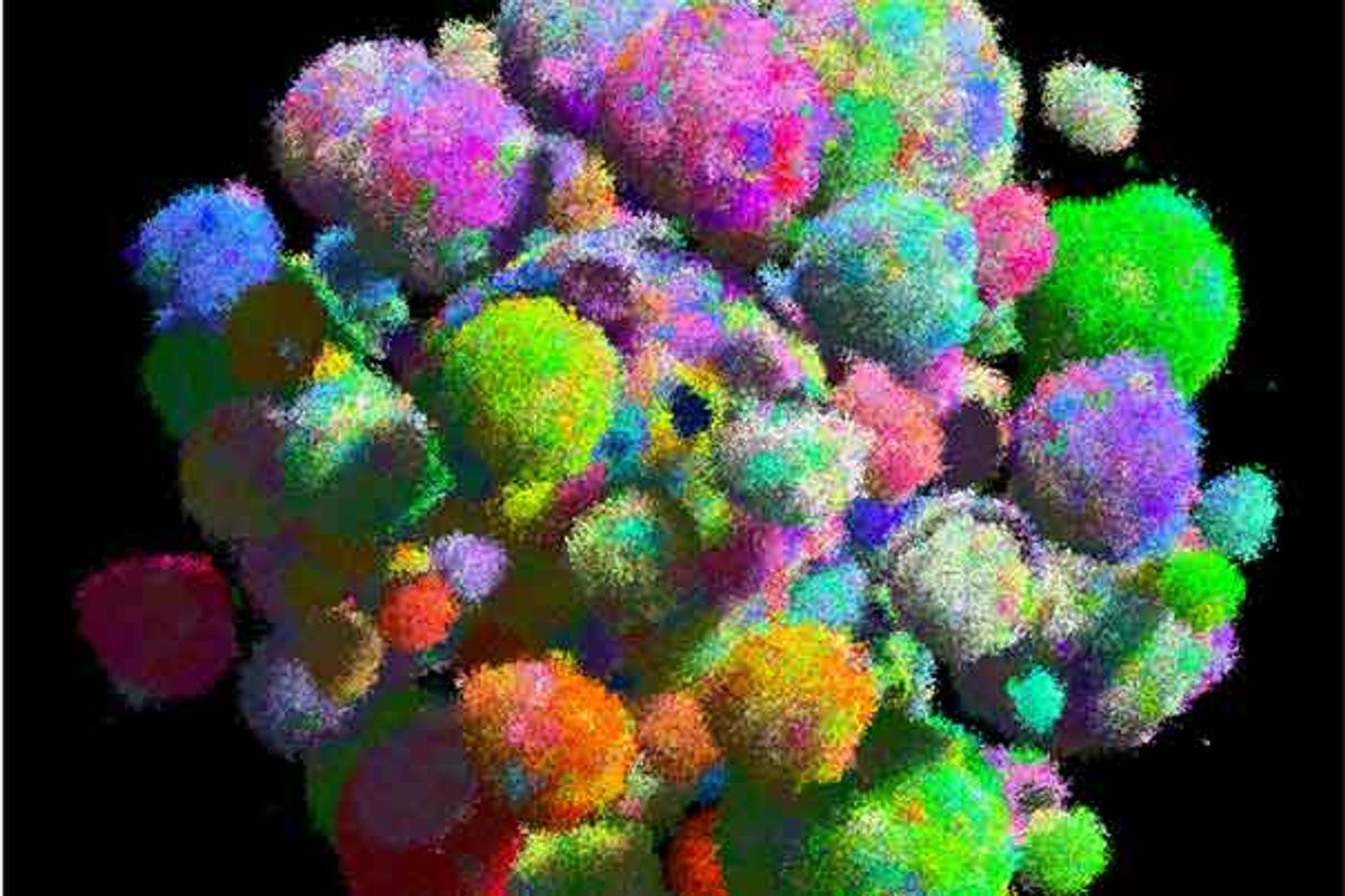
Image Credit: Bartek Waclaw
Models that capture the spatial, or 3-D, aspects of tumors do not reflect their growth speed. Non-spatial models portray the growth of tumors accurately, but not their 3-D nature. The Harvard scientists wanted to unite the two.
A team led by Martin Nowak, director of the Program for Evolutionary Dynamics and a professor of mathematics and of biology, has developed the first model of solid tumor growth that reflects both shape and growth. The study is described in the journal Nature and in
Drug Discovery & Development.
As Nowak explained, “Previously, we and many other people used non-spatial models, but those models couldn’t possibly explain how a solid tumor could arise. Now, for the first time, we have a spatial model that can do that.”
The new model is different. It enables cells to migrate locally and answers critical questions about the proximity of different cells to one another.
Nowak said, “That is what makes cancers grow fast, and it’s what makes cancers homogenous in the sense that cancer cells share a common set of mutations, and what is responsible for the rapid evolution of drug resistance. I further believe that the ability to form metastases, which is what actually kills patients, is a consequence of the selection for local migration. The majority of the mathematical models in the past started with a population of cells, and they would simply count the number of mutations they had, but that’s ignoring the spatial structure, so it doesn’t ask which cell is close to another cell.”
He believes that understanding spatial structure is important, because of the role it plays in how tumors grow. Earlier spatial models, conceived with the idea that tumor cells would divide only if they had the necessary space, produced slower growth, because only the cells on the surface of the tumor could divide. When cells have the ability to migrate locally, “individual cells can always find new space where they can divide,” Nowak said. The result was a model that demonstrates faster growth and explains why cancer cells share a high number of genetic mutations and how drug resistance can develop in tumors.
While all cells develop mutations as they divide, cancer cells have “driver” mutations — changes that enable cells to divide faster, live longer or resist drugs. They cause rapid tumor growth, carry forward passenger mutations and, thus have many mutations in common. Drug resistance happens when cells mutate to resist a particular treatment. Targeted therapies wipe out nearly all other cells, but the few resistant ones quickly replicate, causing a relapse.
Nowak concluded, “This migration ability helps to explain how driver mutations are able to dominate a tumor, and also explains why targeted therapies fail within a few months as resistance evolves. So what we have is a mathematical model for solid tumors, and it’s this local migration that explains these questions.”