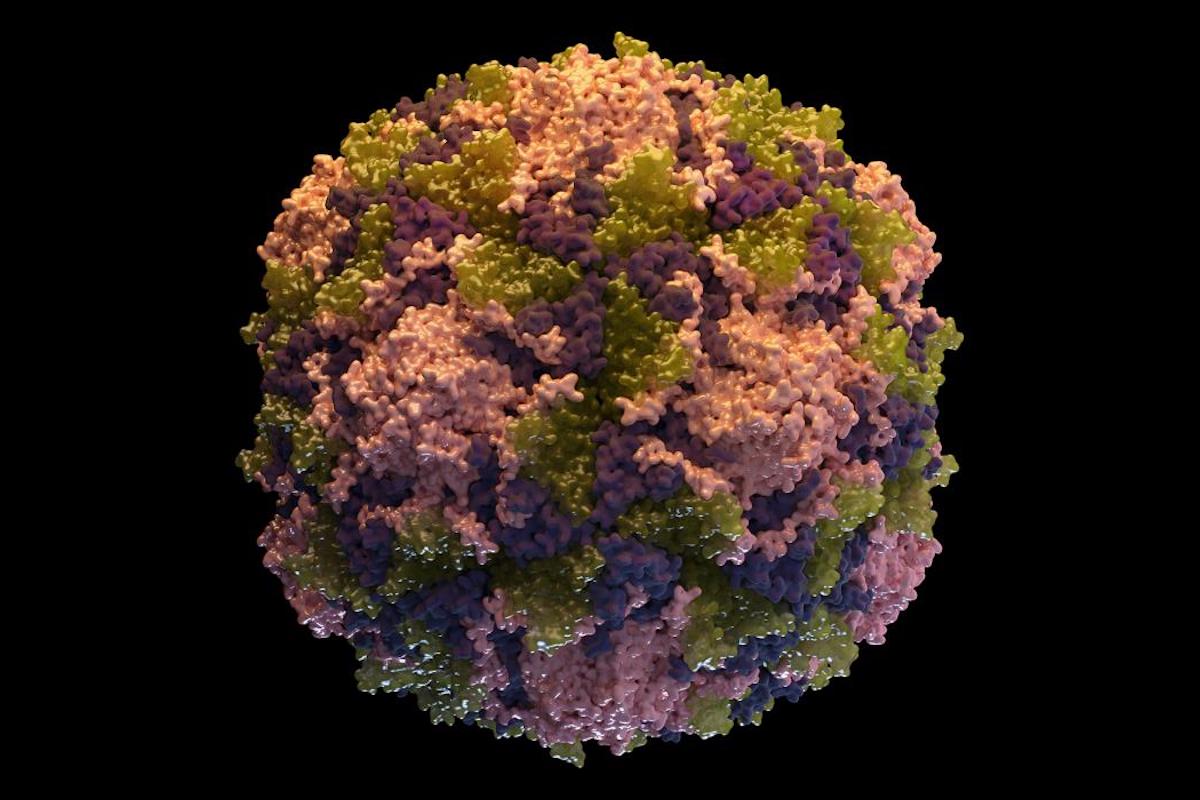
Sustained, intense efforts to vaccinate were getting the world very close to eradicating polio, which is caused by a virus and can cause devastating paralysis. More than 3 billion children have been vaccinated since 2000, and this strategy reduced the disease burden by an estimated 99 percent, and prevented the infection of 13 million children, according to the World Health Organization (WHO). While many lives were improved and saved, there was an unfortunate problem; the weak virus used in the vaccine was able to evolve and caused some outbreaks of polio. The vaccine-derived outbreaks impacted communities in which not everyone was vaccinated and also infected a few vaccinated people too.
The Gates Foundation helped fund an effort to create a new vaccine that would not pose these risks and was designed to be unable to evolve to cause disease. Promising results have come out of the phase 1 clinical trial of the new oral polio vaccine, the first in fifty years.
In 2017, UC San Francisco virologist Raul Andino, Ph.D. and colleagues learned that the poliovirus went through the same three evolutionary changes in every vaccine-derived outbreak they investigated.
Andino and Andrew Macadam, Ph.D. of the UK's National Institute for Biological Standards and Control (NIBSC) and colleagues have now applied that knowledge to decades of research on the polio vaccine, and found a way to make a new vaccine that cannot move through those evolutionary changes. A portion of the viral genome that is necessary for it to infect humans has now been stabilized so that it cannot be modified, even when it exchanges genetic material with other viruses. The work has been reported in Cell Host and Microbe.
"To my knowledge, this is the first effort to rationally design a live attenuated virus based on detailed understanding on its biology, as opposed to the standard approach of blindly passaging the virus in animal cells to eliminate human virulence through poorly understood mechanisms," explained Andino, a professor of microbiology and immunology at UCSF.
In this phase 1 trial, fifteen adults previously vaccinated adults received the newly designed vaccine. The new polio vaccine was found to be more effective and more stable than the one it was made from; plentiful antibodies were generated in the study participants, and the viral particles that were shed in their stool were not capable of infecting mice. The viral particles that are shed in the same way by the previously used vaccine, on the other hand, infect mice and cause around 90 percent to develop paralysis.
A phase 2 trial of the new vaccine is happening now and a phase 3 trial is being planned by WHO, said Andino. They are hopeful that the new vaccine can be fast-tracked for use in outbreaks caused by vaccine-derived polio.
The COVID-19 pandemic has temporarily suspended the polio vaccination campaign, so the Andino lab is studying SARS-CoV-2. They are creating a mouse model to study the spread of the virus and how it causes disease. Andino wants to take a methodical approach that takes advantage of biological pathways in the virus, instead of a quicker route that uses viral particles that may create complications.
"I believe the lesson of polio is that it will take time to develop an optimal vaccine against SARS-CoV-2, and early efforts are likely to meet with unexpected challenges," Andino said. "Once we do have safe and effective vaccines, they'll need to be produced at global scale, which will probably require the use of older technologies that are already in place. Given how little we know about this new coronavirus, I'm betting we'll need all the weapons we can muster."
Sources: AAAS/Eurekalert! via University of California - San Francisco, Cell Host & Microbe

